 In this month’s instalment of the endo expert, Kreena Patel discusses a case using deep margin elevation (DME).
In this month’s instalment of the endo expert, Kreena Patel discusses a case using deep margin elevation (DME).
Subgingival margins are a common clinical challenge. We regularly encounter this situation when restoring endodontically-treated teeth.
The concept of deep margin elevation was first presented by Dietschi and Spreafico in 1998. It gained significant popularity following the paper ‘Deep margin elevation: a paradigm shift’ by Pascal Magne and Roberto Spreafico in 2012.
What is deep margin elevation (DME)?
A direct restoration is used to raise the cavity margin to an equigingival or supragingival location.
Why do we use DME?
Deep subgingival margins are particularly difficult to manage with indirect restorations. The challenges include:
- Isolation
- Impression taking/optical scanning
- Cementation.
Indirect bonded restorations are often chosen because they are aesthetic and conservative to preserve more tooth tissue.
However, they require excellent moisture control during the adhesive cementation procedure. Excess resin cement also needs removing prior to curing, which takes time and has a risk of bleeding when carried out subgingivally.
This can compromise the seal and risk leakage of the restoration long term. Relocating the margin more coronally can help eliminate many of these problems.
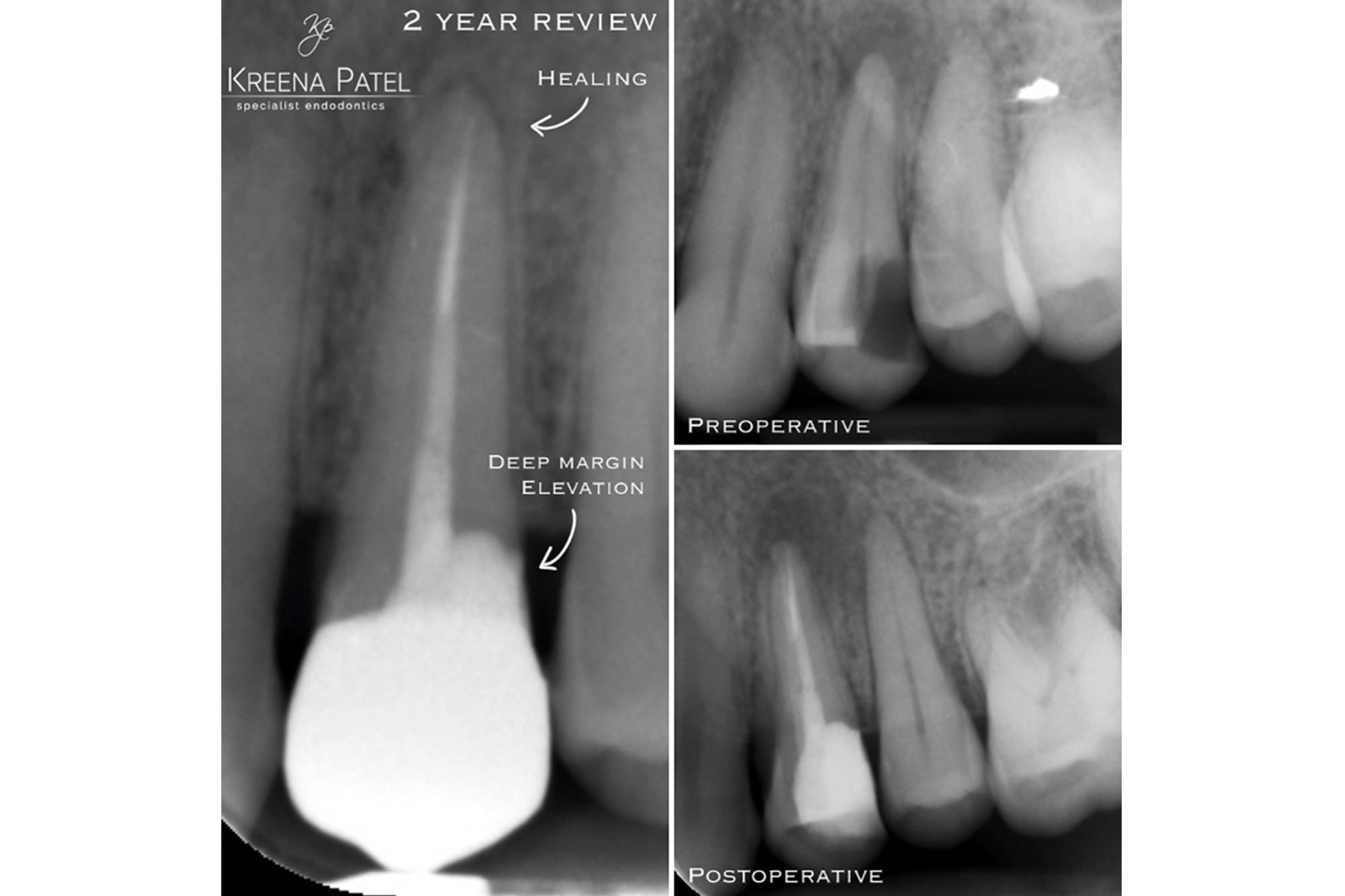
DME allows placement of a rubber dam during the cementation procedure, which can offer more predictable long term results (Figure 1).
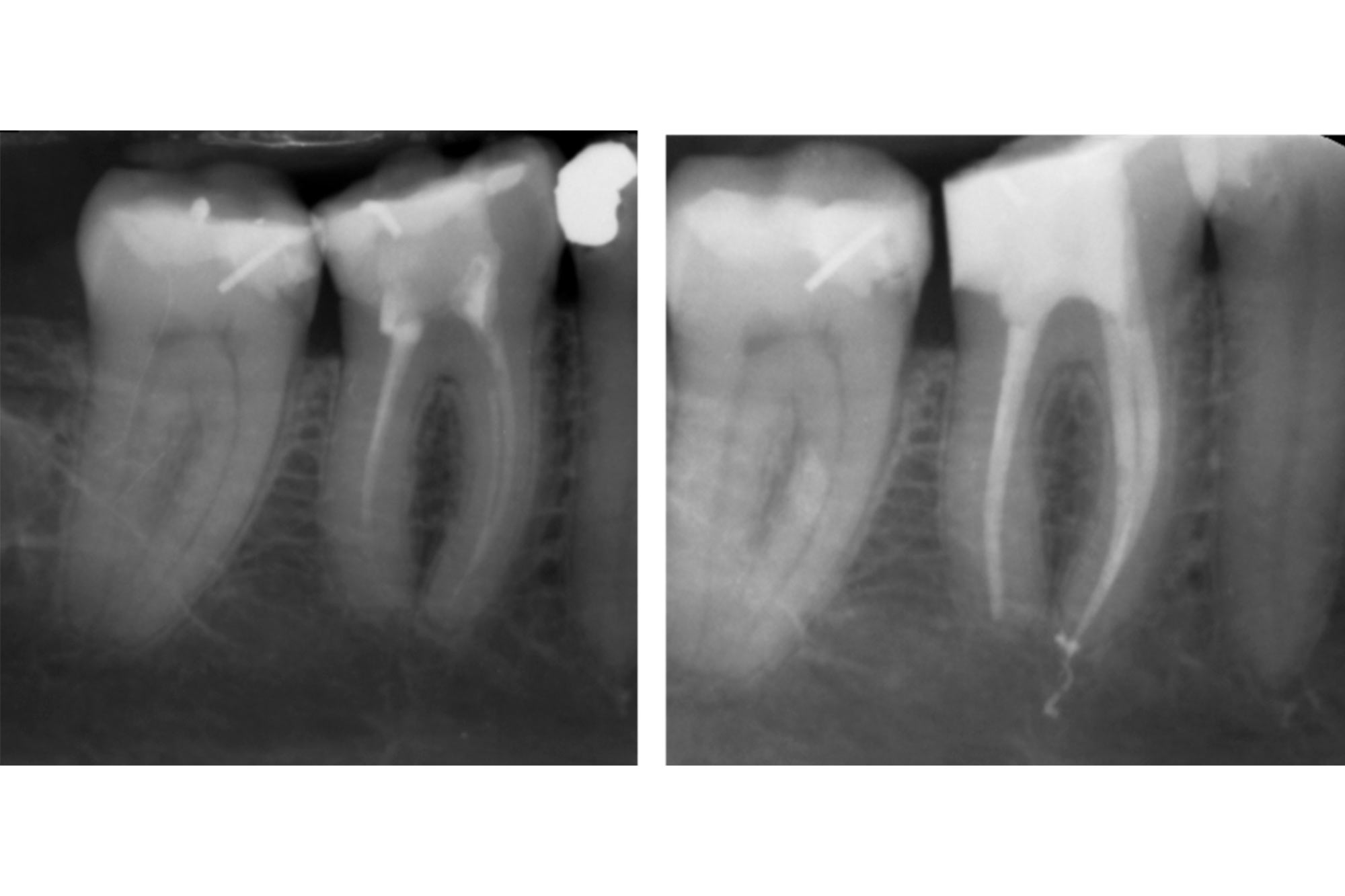
DME is less important when using traditional cements (zinc phosphate or GIC) for non-bonded indirect restorations. These are less technique sensitive, do not require strict isolation and can be removed after the cement has hardened. However, accurate subgingival impression taking still poses a challenge (Figure 2).

Why is it easier to use a direct technique to elevate the margin?
It is easier to place a direct restoration subgingivally. Moisture control is required for a shorter period of time and a matrix system helps achieve this. DME should only be used if a good seal can be achieved.
What are the challenges of DME?
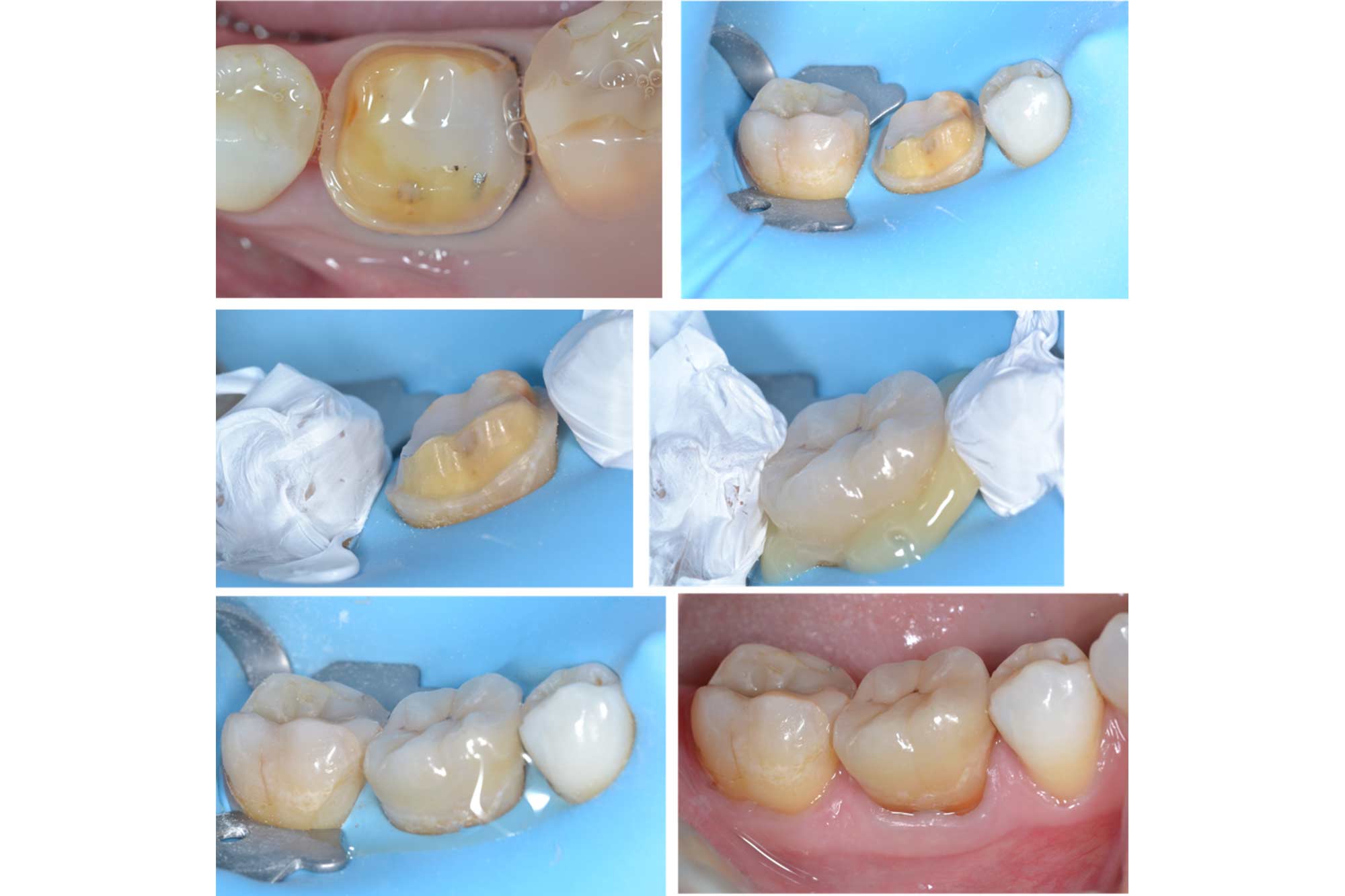
The main challenge for DME is adapting the matrix band to the base of the restoration (Figure 3). Special matrix systems have been developed for this purpose. Regular matrix bands can also be adapted on one side to help the band sit deeper. Wedges, teflon tape, and light cured rubber dam materials (such as Opaldam) are also useful to help achieve a good seal.

When should we carry out DME for teeth requiring endodontic treatment?
It is important to assess if a tooth is restorable prior to carrying out endodontic treatment.
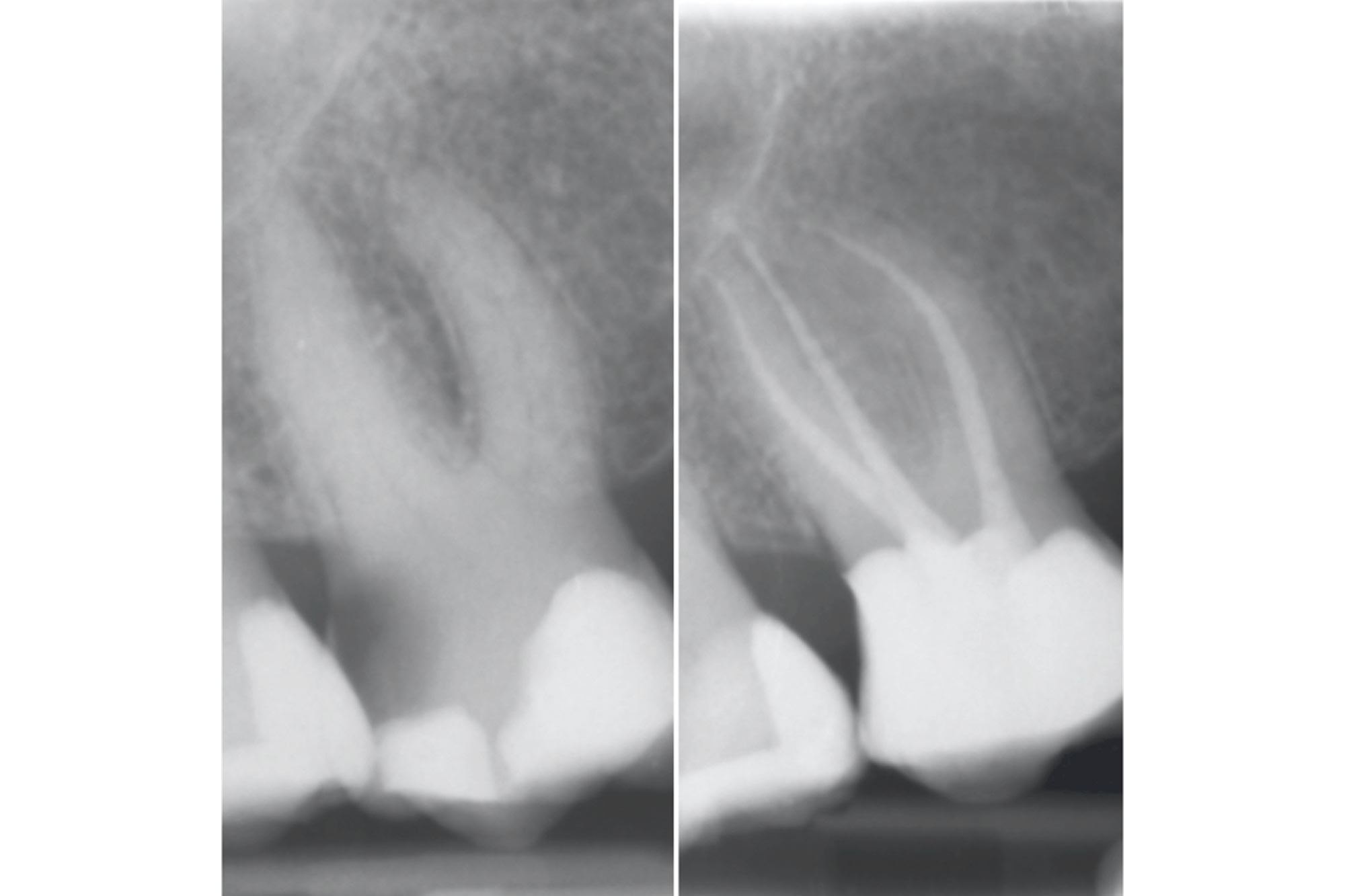
This includes removing any existing restorations and caries, and checking that a well-sealed restoration can be placed. As part of this process the clinician can carry out DME and place the definitive pre-endodontic composite restoration. Following the root canal treatment, the indirect restoration margin can be placed on the composite.
It is not always possible to establish a contact point during the initial build up (Figure 4). Establishing a good contact point at this stage has limited importance because this will be achieved when the definitive indirect restoration is placed.
The most important detail is to remove any material flash to prevent periodontal problems. You can carry this out using a scalpel or fine bur.
If a direct restoration is planned then the contact point will need re-establishing using a sectional matrix system after DME has been carried out.


What material for the direct restoration?
The technique was established using composite resin. An adhesive indirect restoration can be bonded using a resin cement directly to this.
The DME concept can also be applied with amalgam and GIC direct restorations.
A bitewing radiograph should be taken to check the adaption of the restoration for overhangs and deficiencies prior to placing an indirect restoration.
What are the benefits of DME compared to crown lengthening?
Alternatives to DME include surgical crown lengthening or orthodontic extrusion.
Both procedures are expensive and require complex multi-disciplinary care. There is also a time delay for the patient.
Crown lengthening has a surgical morbidity and results in attachment loss. It is not always possible due to anatomical complications (margin location, proximity to adjacent teeth or implants, furcation, root concavities). A patient’s medical history may also limit this option.
Are there any negatives to DME?
There are some disadvantages to DME and it is important to discuss these with the patient prior to starting treatment.
1. Two margins
Ideally the indirect restoration should rest on sound tooth tissue. However, this is sometimes not possible based on the depth of the margin and what material is used.
The restoration is most likely to fail at the deepest margin. The better the seal here – the better the prognosis. A direct restoration can be placed more predictably in difficult situations than an indirect.
Posterior indirect restorations with DME have shown good survival in a study with an up to 12 years follow up (Bresser et al 2019).
2. Biological width invasion
Current evidence shows DME appears to be well tolerated by the periodontium when carried out to a good standard. It has been shown to lead to very few to no signs of clinical inflammation (Safati and Tirlet 2018).
I regularly carry out DME in partnership with my referral dentists, and found the same results.
It is important to advise patients to use interdental brushes regularly to keep the restoration clean and the surrounding periodontium healthy.
Why is it important in endodontics?
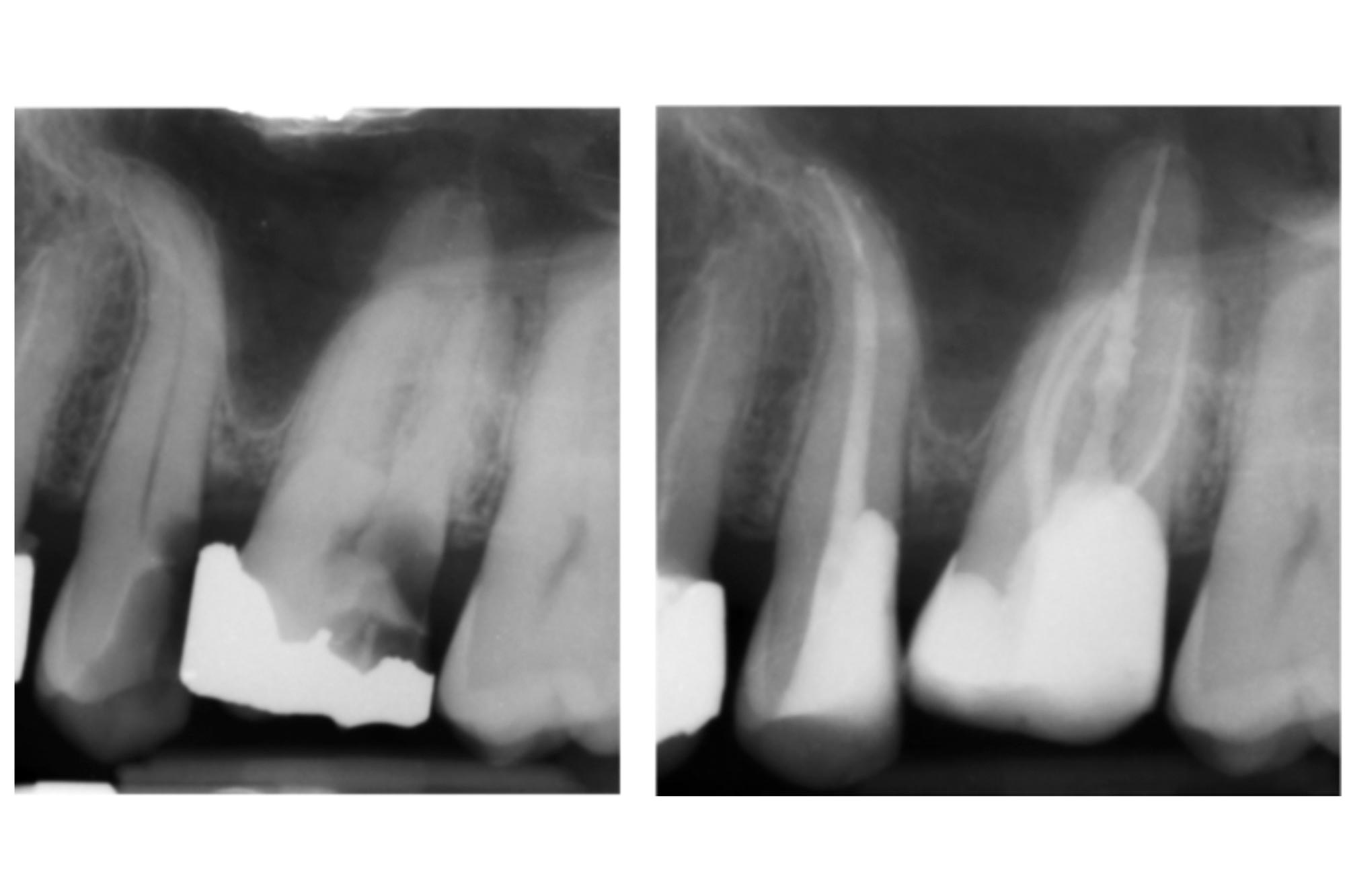
We are often dealing with teeth with subgingival margins in teeth requiring endodontic care. DME means we can save teeth that may otherwise be considered unrestorable (Figure 7).
Restoring these deep margins effectively is usually the most challenging part of the treatment and takes the most clinical time.

Conclusion
DME is a very useful clinical tool and should be used when required. Current evidence shows indirect restorations with deep margin elevation have a good survival rate and lead to very few to no signs of clinical inflammation.
Many of the cases presented are extensively restored. Therefore, naturally have a more guarded long term prognosis. It is important to discuss the benefits and risks with the patient prior to treatment. The importance of regular dental checks and oral hygiene using interdental brushes should be reinforced.
References
Magne P and Spreafico RC (2012) Deep margin elevation: a paradigm shift, Am J Esthetic Dent 2: 86-96
Bresser RA, Gerdolle D, van den Heijkant IA, Sluiter-Pouwels LMA, Cune MS and Gresnigt MMM (2019) Up to 12 years clinical evaluation of 197 partial indirect restorations with deep margin elevation in the posterior region. J Dent. 91: 103227
Sarfati A and Tirlet G (2018) Deep margin elevation versus crown lengthening: biologic width revisited. Int J Esthet Dent 13(3): 334-56
Follow Dentistry Online on Instagram to keep up with all the latest dental news and trends.
If you would like to learn more about endodontics follow Kreena on Facebook and Instagram @kreenaspecialistendodontics.


