Nilesh Parmar launches his new column Implant Insights. To kick start he looks at immediate implant placement to keep up with patient demands.
Nilesh Parmar launches his new column Implant Insights. To kick start he looks at immediate implant placement to keep up with patient demands.
When implant dentistry first became mainstream, the tried and tested protocol of removing the tooth, allowing the site to heal for three to six months, then placing the implant, then waiting another three to six months, before loading, was commonplace.
From a consumer point of view, this was not ideal.
In today’s ‘instant age’, patients are after prompt replacements. They will usually not entertain the idea of a removable provisional such as a denture.
Over time, with development of techniques, drills and improved implant design, we have been moving towards immediate implant placement as a matter of routine.
This has gone as far as removing all of a patient’s teeth and immediately placing implants and a provisional restoration on the same day. Known by marketeers as ‘teeth in a day.’
For the purpose of this article, we will concentrate on the immediate single tooth. Very often we are faced with a fractured or broken down upper anterior tooth that requires removal and implant replacement.
When faced with such a situation we have the following options:
- Immediate implant placement; removal of the tooth and implant placement in the same sitting
- Delayed immediate; removal of the tooth, temporisation of the gap, and implant placement +four weeks later
- Delayed placement; removal of the tooth, temporisation of the gap, and implant placement delayed for at least two to three months.
Delaying placement pros and cons
In many circumstances, delayed placement is unavoidable. If there is a large chronic area of infection, or other issues that would need rectifying prior to implant placement such as acute periodontal disease. Then it may be prudent to delay implant placement until these factors are under control.
Whilst there are clear positives to delaying implant placement in terms of overall implant success, there are downsides, specifically for the patient.
Delayed placement requires increased chair time, further administration of local anaesthetic injections and additional surgical intervention, resulting in time off work or further costs.
The real issue for many patients is the added treatment time. In a world of next-day deliveries and instant online messaging, many patients are surprised when six months is quoted as the timeline to successfully place and restore a single tooth implant.
Added to that delay, we have the issue of how to temporise the missing tooth. A small temporary denture was often the replacement of choice. But there are now various options.
Temporary replacements
- Resin bonded bridge – has the benefit of developing emergence via a gradia pontic, which we can add to during the healing phase. Aesthetics are variable depending on the orientation of the adjacent tooth and skillset of the lab technician
- Temporary partial denture – relatively cost-effective to produce. Simple to fit but with poor patient tolerance, speech and confidence issues
- Immediate temporary crown on immediate implant – this is our ideal situation. It involves tooth removal, with placement of an immediate implant and a tooth affixed onto the implant on the same visit. This requires careful planning and isn’t always possible depending on the bone volume available and the suitability of the site.
Benefits and risks of immediate implant placement
Immediate implant placement has been documented as far back as 1988 by Barzilay et al.
It has the advantage of reducing surgical time, maintaining soft tissue volume and potentially preserving surrounding bone. The extraction socket can also serve as a guide or point of orientation for the surgeon.
There is also the psychological benefit for the patient. Although they are losing a tooth, they are also receiving their implant on the same sitting.
Despite the above, there is also the risk of unpredictable healing, loss of soft tissue volume, difficulty in achieving satisfactory implant stability and ultimately, implant failure.
If we look at the research, there is support for immediate implant placement. Lindeboom, Boticelli and Nemcovsky all reported zero loss of implants after six months follow up with immediate implant placements. These studies all involved lifting a flap at the time of surgery.
A study by Riberiro reports a 7% failure rate of immediate implants. However, these were placed with no flap being raised at the time of surgery.
Factors in case selection for immediate implant placement
Not all cases are suitable for immediate placement. Variables in hard and soft tissues surrounding the proposed implant site will determine which sites are appropriate for immediate placement.
Bone volume is always important in implant placement, not just immediate placement.
One would need to assess if there is sufficient ridge width and height in order to place an implant successfully, with or without the need for guided bone regeneration.
Koh et al have recommended a crest ridge width of 4-5mm and a height of at least 10mm as the minimal dimensions for predictable immediate implant placement.
However, with the introduction of much more aggressive thread design implants, we could reduce these measurements. Other structures, such as the alveolar nerve and the floor of the maxillary sinus may be limiting factors for implant depth as well as width.
Gingival biotype is a key factor in immediate implant placement, especially in the aesthetic zone. Patients with thick gingival biotypes have a reduced risk of gingival recession following on from surgical intervention. Those with a thin biotype have an increased risk of poor aesthetic outcomes, especially in high smile line cases.
The presence of chronic infection has long been an absolute contraindication for immediate implant placement.
However, studies by Lindeboom et al have shown thorough debridement and cleaning of the osteotomy site, as well as administration of antibiotics prior to implant insertion, can result in comparable success rates to delayed placements.
This is dependant on adherence to thorough disinfection protocols and close monitoring of the implant site post insertion.
Conclusion
In conclusion immediate implant placement is challenging and technique sensitive for the operator.
It would be recommended, that this treatment modality is of the more ‘complex’ implant treatment provision with case selection a key criteria in a successful outcome.
Implant type and design appears to be a factor in immediate implant insertion. With certain implants better tailoring to this protocol.
Case study
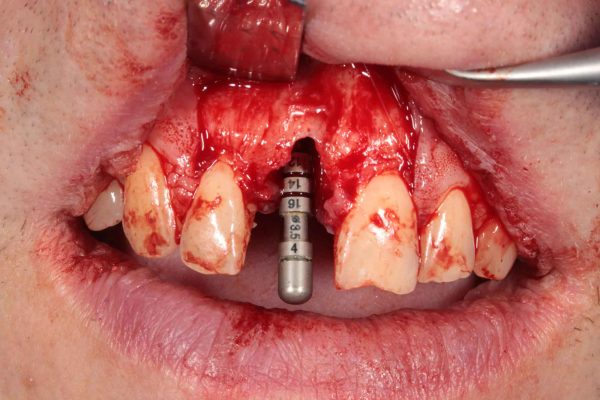
Mr A presented with a longitudinal root fracture associated with the post-treated UR1 incisor tooth (Figure 1).

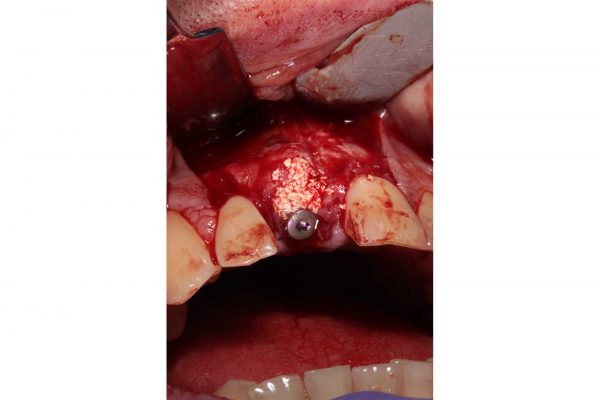
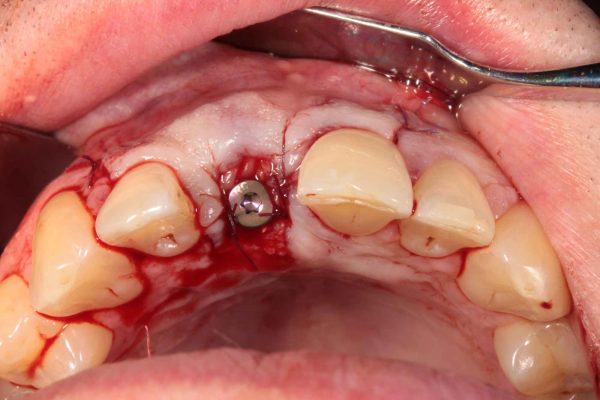
The UR1 was removed and an immediate Straumann BLT implant with an associated bovine graft (Cerabone) with a PRGF plasma fibrin (BTi) membrane placed at the time of implant surgery (Figures 2-8).
Healing occurred without incidence. After an integration period of three months, the implant was restored with a screw-retained restoration.
Mr A was taking oral bisphosphonates. So a regular monthly review was carried out post-surgery to assess healing.
Figure 9 shows a two-year follow-up showing healthy peri-implant tissues with apical migration of mesial papillae.

Follow Dentistry.co.uk on Instagram to keep up with all the latest dental news and trends.