Anna Middleton considers how biofilm interacts with whole body health, and what can be done to help patients achieve a cleaner mouth and therefore a potentially healthier body.
As dental professionals know all too well, oral biofilm has the potential to contribute in no small part to dental diseases.
Indeed, robust evidence indicates that biofilm in dysbiosis can trigger caries and periodontal diseases, leading to symptoms and outcomes such as bleeding gums, bad breath, gum infections, receding gums, and ultimately, tooth and implant loss.
Patients are certainly aware of some of these issues, especially when pain and sensitivity come into play. That’s when the non-regulars tend to seek help from their dentist, dental hygienist or dental therapist.
However, there is a marked lack of awareness of how oral conditions can have health repercussions far beyond the mouth.
Systemic diseases
The evidence in this area is increasing and ongoing, so no definitive path or solution is available for us yet to share with patients.
What we do know so far is that bacteria in oral biofilm find their way deeper into the body and links have been shown to exist between dental diseases and other inflammatory conditions over time. For instance, studies have found that oral biofilm may lead to diabetes as well as cardiovascular disease.
In fact, at least 57 systemic conditions have been hypothesised to be linked with periodontal disease, although there are varying levels of evidence at this point (Monsarrat et al, 2016; Winning and Linden, 2017).
Some of the more commonly encountered potential areas of concern include:
- Depression
- Cancer
- Lung disease
- Liver disease
- Premature birth
- Stroke
- Rheumatoid arthritis.
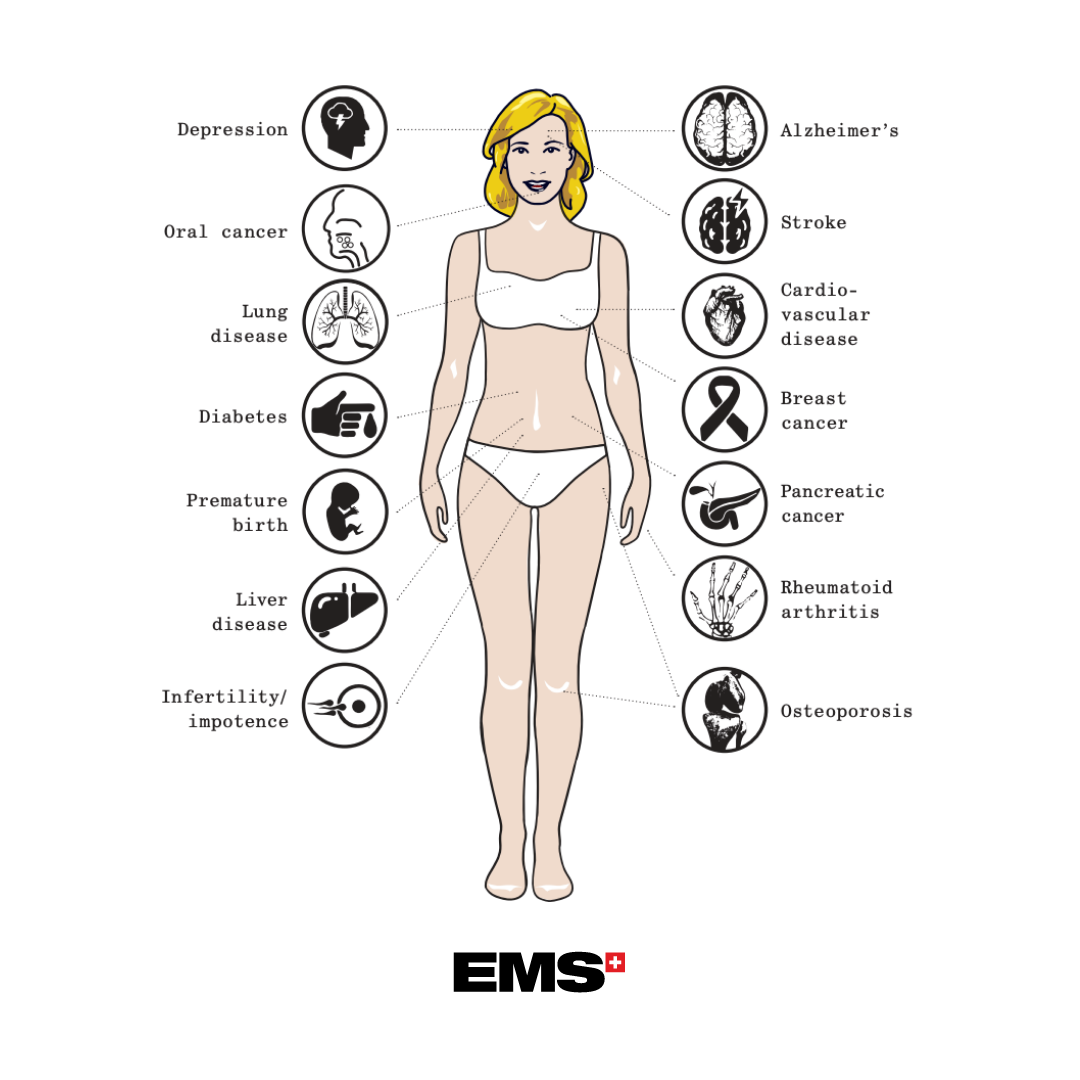
To reiterate, the caveat here is that the evidence base is evolving in all these areas. Nonetheless, as written in the Royal College of Surgeons’ position statement, ‘The evidence … suggests that [oral health professionals] could potentially play a broader role in supporting patients’ general health, both by helping to diagnose certain wider health problems and by providing healthy lifestyle advice.’
Biofilm is neither ‘good’ nor ‘bad’
There can be a tendency to over-simplify biofilm as being either ‘good’ or ‘bad’, but the truth is that defining it that way misses certain important aspects of the process that lead to disease.
As Marsh (2012) wrote: ‘…in contrast to many situations in medical microbiology, it is too simplistic to talk of the presence of ‘good’ or ‘bad’ bacteria. Disease is a result of undesirable changes to the microbial balance, metabolism, and composition of these dental biofilms.’
Therefore, what is need are appropriate plaque control strategies to reduce the prevalence of dental disease, which may well then serve to benefit individual patient’s overall health over the long term.
Why innovative care is needed
The upshot of all of this is that oral biofilm must be removed – on a regular basis, without pain, gently and effectively.
The gold standard of home care remains brushing twice a day with a fluoridated toothpaste, spitting and not rinsing with water, and interdental cleaning daily, alongside any other personalised recommendations by a dental professional.
This is the ideal accompaniment to professional prophylaxis, but it is time to move beyond ‘traditional’ scaling and polishing.
A study conducted by Germany’s Stiftung Warentest (a consumer advocacy foundation) revealed significant shortcomings in conventional professional tooth cleaning.
This study indicated that the method using brushes, polishing paste and hand-held instruments only removes 50% of biofilm in areas that are difficult to reach. In addition, the lack of a common clinical protocol contributed to major differences in terms of results.
This was later confirmed by a Cochrane publication (Lamont et al, 2018), showing that traditional professional teeth cleaning is not able to prevent oral diseases: ‘For adults without severe periodontitis who regularly access routine dental care, routine scale and polish treatment makes little or no difference to gingivitis, probing depths and oral health‐related quality of life over two to three years follow‐up when compared with no scheduled scale and polish treatments (high‐certainty evidence).’
Clearly, there is room for improvement beyond the traditional approach.
The game-changing solution for biofilm
A newer protocol gaining traction worldwide is that of guided biofilm therapy (GBT). GBT is an evidence-based, indication-orientated, systematic, modular prevention for prophylaxis and a therapy protocol for all dental applications.
It is given in the least invasive way, with the highest level of comfort, safety and efficiency, achieving optimal results. This pleasant and comfortable experience will motivate patients to return for regular recall visits, ensuring effective upkeep.
All in all, GBT represents a paradigm shift in dental hygiene, and will no doubt earn its place in the evolution of preventive oral care, as more and more dental professionals and patients become aware of what can be achieved with it in the right hands.
The GBT protocol in eight simple steps
- Assess – probe and screen every clinical case
- Disclose – make biofilm visible
- Motivate – raise awareness and teach
- AirFlow – remove biofilm, stains and early calculus
- PerioFlow – remove biofilm in >4 to 9 mm pockets
- Piezon No Pain – remove remaining calculus
- Check – make your patient smile
- Recall – a healthy patient equals a happy patient.
References
Lamont T, Worthington HV, Clarkson JE, Beirne PV. Routine scale and polish for periodontal health in adults. Cochrane Database Syst Rev. 2018 Dec 27; 12(12):CD004625. doi: 10.1002/14651858
Marsh PD. Contemporary perspective on plaque control. Br Dent J. 2012 Jun 22;212(12):601-6. doi: 10.1038/sj.bdj.2012.524
Monsarrat P, Blaizot A, Kemoun P, Ravaud P, Nabet C, Sixou M, Vergnes J-N. Clinical research activity in periodontal medicine: a systematic mapping of trial registers. Journal of Clinical Periodontol 2016; 43: 390-400. doi: 10.1111/jcpe.12534
Royal College of Surgeons Faculty of Dentistry position statement 2019. https://www.rcseng.ac.uk/-/media/files/rcs/fds/media-gov/fds-position-statement–oral-health-and-general-health-final-v4.pdf
Stiftung Wahrentest, test 7/2015. Professionelle Zahnreinigung, Gesundheit, p86-89
Winning L, Linden GJ. Periodontitis and Systemic Disease: Association or Causality? Curr Oral Health Rep. 2017; 4(1): 1-7. doi: 10.1007/s40496-017-0121-7.
If you would like further details about GBT, please visit www.ems-dental.com.


