This month Richard Jones, a specialist orthodontist at Total Orthodontics, part of Bupa Dental Care, discusses the often overlooked role that orthodontics can help play in managing distressing situations for young patients.
At some time in our careers, almost all of us have been or will be presented with a situation in which a traumatised child presents at the surgery with significant dental trauma. Perhaps it involves intruded, luxated or avulsed teeth.
These can be some of the most challenging clinical situations we face, which constitute genuine emergencies.
As well as our role in calming distressed patients and parents, our clinical decisions at these times can have a profound effect on the long-term outlook in both health and aesthetic terms and impact a child positively or negatively for the rest of their lives.
This month’s column discusses the often-overlooked role that orthodontics can help play in managing such situations and may just help you save a smile.
Easier said than done
In terms of acute management of intrusive and lateral luxation injuries of teeth involving alveolar fractures, the International Association of Dental Trauma (IADT) and The British Society of Paediatric Dentistry (BSPD) both recommend repositioning the teeth digitally or surgically under appropriate anaesthetic, followed by splinting. This is if spontaneous eruption is unlikely.
This is the approach we are all most familiar with.
However, this is often easier said than done. And it can often prove difficult, if not impossible, to reposition the teeth accurately, especially if there is bony comminution or healing if some time has passed since the injury.
Less often reported or utilised, but also contained within the recommendations, is the use of orthodontic treatment to reposition intruded or luxated teeth and simultaneously splint the teeth.
The potential benefits of using adjunctive orthodontic treatment to manage the acute situation include:
- More accurate repositioning of the teeth
- Potentially a less traumatic experience for the patient than surgical/digital repositioning
- Ease of splinting (which is provided by the appliance)
- Potentially better bony contour.
On the other hand, the potential disadvantages include a possible delay to pulp extirpation and RCT. This may occur in cases where rapid pulp extirpation is deemed necessary to help reduce the risk of complications, such as inflammatory root resorption.
An unfortunate skiing accident
This real-life case of mine demonstrates this process in action to achieve an outcome that would have been hard, if not impossible, to achieve any other way.
This unfortunate patient was actually nearing the end of orthodontic treatment when she suffered a freak ski accident in France.
During a fall, her ski pole stopped firmly and suddenly followed by her teeth which hit the top of the pole with huge momentum.
It is probably fair to say that if it hadn’t been for the fixed appliance in place, quite a number of teeth would have been avulsed (Figure 1).

Sadly, emergency services at the resort could not help much in managing the problem. A CT scan revealed the extent of damage to the alveolus, which was significantly comminuted in places. Although, thankfully, no roots were fractured.
She was packed onto a plane and came to see me less than 24 hours later.
What to do?
The injuries were significant with the intrusion of UR123, lateral luxation injuries of UL1 and the entire lower labial segment. All of which had been displaced lingually from the direction of the force.
She now had a significant reverse overjet. The UR2, in particular, was highly mobile and barely visible, swimming in shattered alveolar bone and blood clot.
Digital or surgical repositioning of the teeth seemed completely impractical. But healing the teeth in these positions would be catastrophic in the long term, especially with the risk of ankylosis.
Initially, under local anaesthetic, the rigid stainless-steel wires were removed. The level of distortion to these rigid wires can be seen in Figure 2.
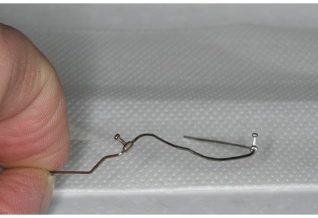
The UR2 was barely visible, but a light 0.016-inch heat-activated niti wire was placed in the other teeth. This rapidly started to reposition the teeth and alveolar fragments while simultaneously providing flexible splinting.
Within a week, the soft tissue trauma had settled, and the UR2 was visible but highly mobile with no tangible alveolar support.
The tooth was splinted to the neighbouring UR3 with a small section of wire to allow some bony healing. After another two weeks, a very light wire was placed into the bracket, and the tooth began to align.
In all likelihood, the UR2 was moving through a form of osteogenic distraction rather than normal tooth movement.
Saving a smile
Within two months, we had almost returned the teeth to the position they were in pre-injury (Figure 3).

We worked closely with our local paedodontic colleagues, and two teeth required RCT around this time.
By four months, we were able to remove the appliances (Figure 4).

The UR2 could not be fully aligned and likely stopped moving once the bone healed and has now ankylosed.
There are some uncertainties about the future and perhaps some teeth will suffer from resorption in due course. However, with the teeth all in a favourable position, there will be lots of decent restorative options with well aligned teeth and good bone volumes.
So, never underestimate the power of your skillset as an orthodontist to help save a smile.
Read previous Total Orthodontics columns:
- Extracting poor prognosis first molars in mixed dentition
- What are fixed functional appliances?
- The ins and outs of DIY orthodontics
- IPR is nothing to fear.
Follow Dentistry.co.uk on Instagram to keep up with all the latest dental news and trends.



