 Dental Protection analyse UK dental orthodontic cases and claims relating to root resorption in child orthodontic patients.
Dental Protection analyse UK dental orthodontic cases and claims relating to root resorption in child orthodontic patients.
Dental Protection’s philosophy is to support safer practice in dentistry and to help members avoid problems arising in their professional practice.
One of the many ways we look to support members in reducing risk is by sharing insights from our cases and claims. This will help clinicians understand how problems may arise. Most importantly, they will understand how they can prevent them in the first place.
Data sources
As part of our ongoing commitment to share learning and insight from cases, Dental Protection has been developing systems to assist in the analysis of unstructured data contained within case files.
Data extraction
One of the outputs of this work is the production of a risk dashboard. This supports the identification of common themes in the cases we deal with.
Further development of these analytical tools will enable us to identify themes and trends in cases more efficiently. In turn, this will allow us to share more information with members about risks arising in different areas of practice.
This is the first Dental Protection article that uses unstructured data analysis software to support the claims review.
Data synthesis
A review of claims data was undertaken focusing on claims relating to orthodontic care. Dental Protection opened these during the period 2016-2020.
For the purposes of this article, the claims in the analysis were those involving patients who were aged 18 or under at the time the first alleged failings in care arose.
The claims reviewed relate to treatment provided by both specialist orthodontists and non-specialists practitioners.
Conclusions
Out of the total claims in this data set, approximately 10% had allegations related to root resorption.
Of note, claims involving root resorption feature more strongly in our higher value orthodontic claims (see Figure 1).
Root resorption claims
Root resorption is a recognised risk associated with orthodontic treatment. There are potentially significant long-term consequences for the patient.
Therefore, it is not surprising that a proportion of the higher value orthodontic claims we deal with will involve root resorption.
In most of the child root resorption cases reviewed, common factors were noted. These factors may have made the patient at higher risk of teeth being affected by root resorption:
- Ectopic/unerupted canines (47%)
- History of trauma prior to commencing treatment (24%)
- Root shape (eg blunt root apices) (12%).
We should note that in the cases involving ectopic/unerupted canines, just over one third of the cases relate to delays in referral for orthodontic treatment.
In these cases, root resorption already occurred before any orthodontic treatment was considered or provided.
The importance of monitoring the development and eruption of maxillary canines was the subject of a previous Dental Protection article ‘Ectopic canines – dentolegal challenges and how to avoid them‘.
Common themes in claims involving root resorption
It is expected that patients for whom orthodontic treatment is being considered should routinely be made aware of the risk of root resorption as part of the consent process. This is a recognised risk of orthodontic treatment.
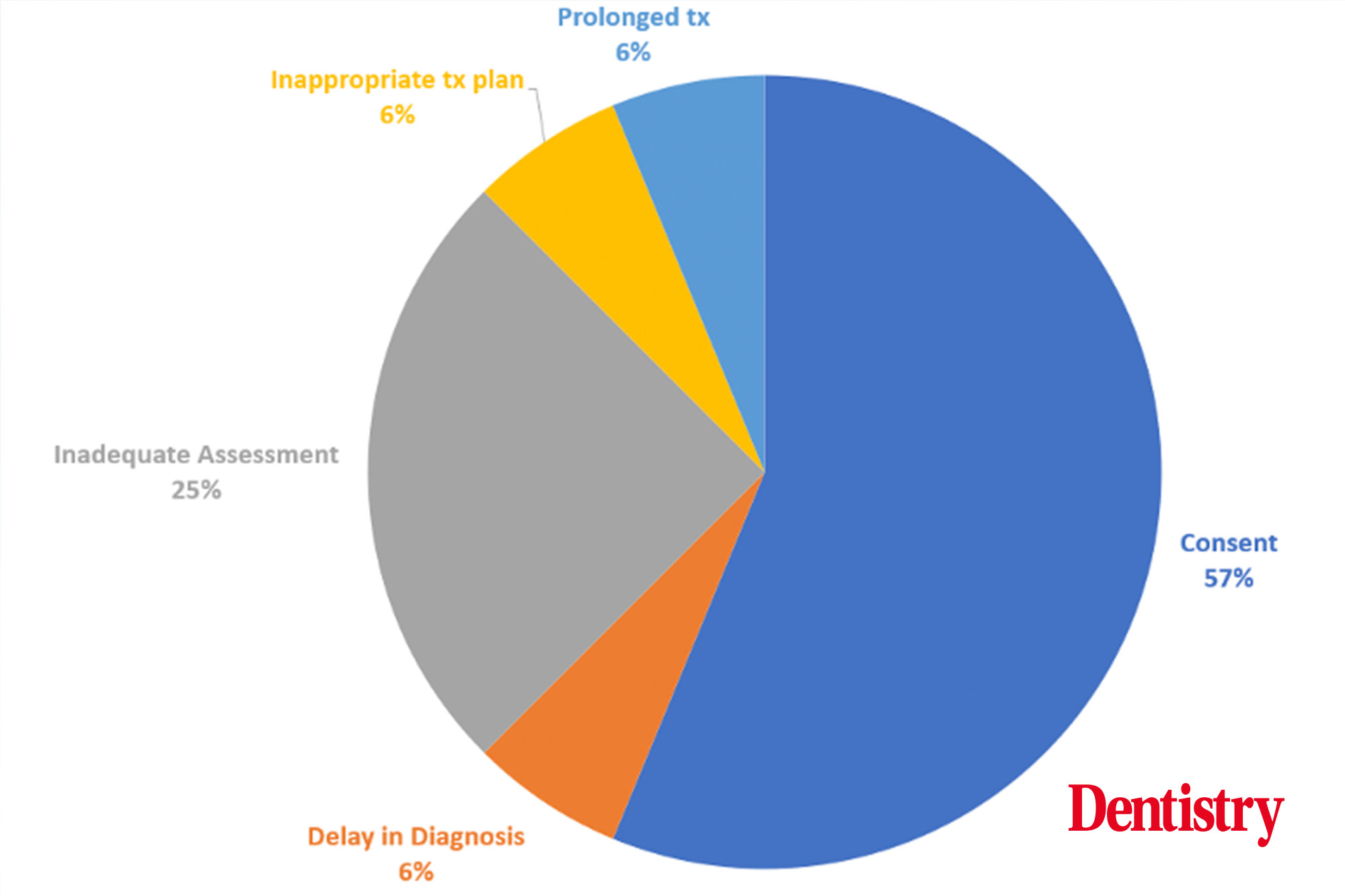
Therefore, it is surprising to see that in over 50% of the claims reviewed, alleged failings in the consent process were a dominant factor.
Figure 2 below shows the main alleged failings in the claims reviewed.
In many of the cases, predisposing factors were present. This may make the patient at greater risk of root resorption.
To defend a claim of this nature, it is important for the records to demonstrate that:
- The increased risk was identified
- Specific risks that a particular patient faces are discussed and understood by the patient
- The treatment plan was appropriate
- There was consideration of alternative ‘lower risk’ alternatives, as well as communication with the patient
- There was appropriate monitoring of teeth during treatment.
Experts will invariably opine on the above. These are the points on which claims involving root resorption may succeed or fail.
Inadequate monitoring
Sometimes predisposing factors could be present and the records only provide evidence that a patient is provided with generic information about the risks. It is unlikely the warnings will be found to be sufficient to demonstrate that consent to treatment was valid.
Where a patient is successful in their claim, damages are significant. For a young patient, tooth loss may result in damages to cover a lifetime of implant placement and restoration cycles. As well as reflecting the psychological impact.
The issues in Figure 2 were not the sole issues arising in the cases. Additional allegations relating to inadequate monitoring, prolonged treatment and poor outcome were the most common secondary factors.
In around a third of the cases where predisposing factors were noted, secondary allegations were made. These stated that there had been inadequate monitoring of the teeth during active treatment.
When considering these allegations, experts will comment on whether monitoring was in line with any guidance and teaching.
Where there is a lack of consensus, experts will assess the case on whether the approach was reasonable at that time.
For those treating patients with a known history of trauma, guidance such as that by Sandler et al (2021) would be of relevance. It also may be relied upon by experts in future.
Allegations relating to consent, assessment and monitoring were common themes across both specialist and non-specialist practitioner groups.
Risk prevention
Orthodontic treatment is not without risk and for some patients the risks of treatment may outweigh the benefits. Ultimately the decision on whether to proceed with orthodontic treatment rests with the patient.
They must make this choice based upon balanced and objective information that has been shared by the treating clinician. This will help a patient understand the risks.
Identifying that significant root resorption has arisen is not only distressing for the patient. This is because it also generates significant anxiety for the clinician who has treated the patient.
However, it is important to remember that this finding will not necessarily result in a patient making a complaint or claim. Additionally, they are less likely to do so if they had understood and accepted the risk of this arising at the outset.
Similarly, being the subject of a claim does not mean that the claim will need to be settled. In most of the cases we see, the successful defence of claims relating to root resorption will rely heavily upon the details within the records. This will demonstrate that the consent was valid and clinical treatment was appropriate.
A guide to avoid root resorption cases
As a general guide, the following checklist may help in the defence of a claim. But perhaps more importantly, it will avoid a patient going down this route in the first place:
- Ensure that any orthodontic assessment routinely includes an assessment of any potential risk factors for root resorption. Also, ensure it documents both positive and negative findings
- Where the assessment identifies a patient may be at a higher risk of root resorption, ensure that the records reflect the specific risk that patient faces. Also, ensure they reflect whether alternative treatment options, including no treatment at all, were discussed
- Where risks are increased, ensure that any written information provided to the patient is tailored to reflect the identified increased risk
- If it is proposed to monitor root health during treatment with radiographs, ensure that a clear note is made in the records as part of the treatment plan as to when any radiographs should be taken. This is particularly important in settings where a patient may be seen by multiple clinicians or where care is being transferred
- In the event root resorption is identified, it is important to be open and honest with patients and ensure that not only is the presence of the root resorption discussed but also what steps may be necessary to mitigate any further exacerbation of the problem. Before continuing with further treatment, the consent process should be revisited, and records updated to reflect the discussions and options discussed
- In the event teeth are subject to trauma after treatment has commenced, ensure any assessment and ongoing treatment reflects contemporary guidance and teaching. It is important to also revisit the consent process, to ensure the patient is involved in any further decision making, and aware of the risks and alternative options.
‘We’re not following a trend’ – trans inclusivity in dentistry
 Dental therapist Leon Bassi talks us through the importance of supporting the trans community and why this will make dentistry a better profession.
Dental therapist Leon Bassi talks us through the importance of supporting the trans community and why this will make dentistry a better profession.
Why did BSDHT make a stand on the trans community?
It was prompted by the Black Lives Matter (BLM) protests but even prior to that we were discussing diversity and inclusion in some fashion. The BLM protests brought it to the forefront of the agenda.
We’ve now formed the advisory group on diversity, inclusion and belonging (DIB). Part of that is to make sure we’ve got our finger on the pulse and to make sure we’re an inclusive rather than an exclusive society. We have such a diverse membership within the British society of Dental Hygiene and Therapy, so we knew this would benefit all of us.
We recently spoke out in support of the trans community; I think that community in particular is such a vulnerable one, especially with all the discussions around banning conversion therapy for all LGBTQ+ people and the issues surrounding teenagers who are wanting to transition.
Make people heard
It’s such a unique issue but we know some people are often scared to talk about it or they may not be in a position where they can talk about it. I think we just want to make sure everybody has a level of audibility. That they’re not just being heard, but we’re also actively listening to them.
We also want to absorb what’s being spoken about so that’s where the diversity, inclusion and belonging group comes in. It’s about making these people who are often not heard, heard.
We have a platform where it might not necessarily be a direct issue with all people. But it will affect all members of the workforce and will affect how we receive patients. It’s very difficult for people who are at different stages of transitioning to access oral healthcare, for example.
Even just a small post on Twitter or on Instagram can give all health care professionals a little window of knowledge when it comes to treating those on this journey.
Charities also do a good job of this – Stonewall have got a campaign to make sure you know about banning conversion therapy. Another charity, AKT, do a lot with LGBTQ+ youth homelessness, which in turn inevitably affects those who identify as trans.
Have there been some difficult conversations to navigate?
I don’t think we’ve had any difficult conversations. The DIB advisory group has been well received. We’ve had no negative narrative given to us from non-members on our posts or tweets.
I think sometimes it’s making sure these things aren’t seen as novelty. For example, the rainbow lanyard is quite key for somebody who is LGBTQ+. But we’ve got to make sure these things don’t turn into novelties – that those wearing it really understand why we’re wearing it and why somebody from the trans community might identify with it and feel they can be more open about their health.
I think health issues, social issues, and just issues surrounding the trans community are so unique so it’s about making sure things are there to support people from LGBTQ+ communities.
We want people to know we are not ticking a box and we’re not following a trend, but this is a meaningful conversation and we want to make sure our audibility is authentic and genuine.
In regards to the trans community, myself and other members of the group have had these discussions. We’re looking at these issues over the long term, not just the short term. We want to promote a culture that everyone is invested in.
How many people actually know a trans person? We know that person does not just wake up one day and think ‘I want to transition’ as such – it can be a harrowing journey and we have to acknowledge that.
When it comes to gay pride – for example, in London – there’s lots of discussions about how it is too commercial. Do people actually know where it originated from? Are they familiar with the Stonewall riots?
According to the most recent GDC statistics, only 1% of dentists identify as a gay man or bisexual, with none identifying as a gay woman. For DCPs, the figure is 1%. What are your thoughts on this?
In terms of these statistics, I don’t think it is a true representation of the LGBTQ+ community within dentistry. It begs the question are we asking the right questions?
I think it starts at dental school and the university system itself. Is there enough representation? We can’t teach students everything but are they taught enough about it? Is there enough research into LGBTQ+ people accessing oral health services?
The narrative around it is so polarised with trans people. But approaches need to be evidence-based and factual. For example, when you consider teenagers transitioning, look at the evidence – it doesn’t match some of the narratives thrown around. I think as healthcare professionals especially, we’ve got to look at the evidence and not the discussion on social media.
We should seek advice from key stake holders, such as charities and foundations, who are looking at the evidence and help gain appropriate patronage so those in government can be accessed and are aware of the issues.
This will enable long term support which can be put into place to support the LGBTQ+ community. What we need to do is make sure our discussions are evidence-based on the topic rather than personal opinions. That’s how we should support people who are transitioning. A language that is inclusive, not exclusive, is the way forward.
Is there anything practical that practices can do?
With the DIB advisory group, it’s all quite new. We’ve recently carried out a survey of members. We plan to publish the results in the Dental Health, the Journal of BSDHT.
However, there are more practical efforts such as the use of pronouns, for example. I teach at a university and I think pronouns are a good way of signalling to other people that you’re comfortable to discuss those things.
I think some people see pronouns as, ‘there they go again’ and see it as a tick box exercise. If they are used authentically, I think pronouns can really help people and create a discussion. I’m very pro people using their pronouns and it’s on our radar for the DIB advisory group.
It’s these small, genuine actions – which might look like a fashionable accessory to an email signature – but to somebody thinking about transitioning, for example, it signals that this person might have an understanding or be open to a discussion.
Distance to go
I’m part of an LGBTQ+ group at university. It’s a great way to make sure people, executive committees, and those in positions of influence are fully aware of the issues faced by LGBTQ+ people in the workplace.
For some reason people think it’s now always accepted but in certain segments of society we’re still not having acknowledgement.
If you look at the recent government decision not to ban all gay conversion therapies, this signals that we’ve still got so much distance to go.
I’m only 40 but I was at school when Section 28 was still part of the education system. I was educated in a system which did not acknowledge my existence in terms of what they classed as ‘normal’.
The charity Mermaids write on their website that they help gender diverse kids and families. It’s simply a level of diversity – it just means, ‘I’m just on a different level of the spectrum’. We’re all on a spectrum – I’m just sitting at this point and you’re sitting at another point.
Follow Dentistry.co.uk on Instagram to keep up with all the latest dental news and trends.


