
Dental hygienist Sakina Syed discusses the link between oral health and menopause, and how dental professionals can help patients experiencing oral-related symptoms.
The importance and awareness of oral microbiomes are increasingly being raised in general health these days, which fortunately in turn also raises the importance of oral health. However, the mouth is the gateway to the body, and we should be seeing the mouth and body as one entity.
The New Scientist International Edition wrote a great piece in December that discusses recalibrating the mouth and body, highlighting that that oral cavity harbours over 500 different oral microbiomes – the second most abundant site than the gastrointestinal tract.
We are aware that the link between poor oral health and systemic diseases is bidirectional, such as cardiovascular disease (CVD), diabetes and Alzheimer’s, and menopause in some ways is no different. It may not be systemic, but it is inflammatory-linked, and women do report oral-related symptoms – we just do not talk about the ‘M’ word.
The ‘M’ word
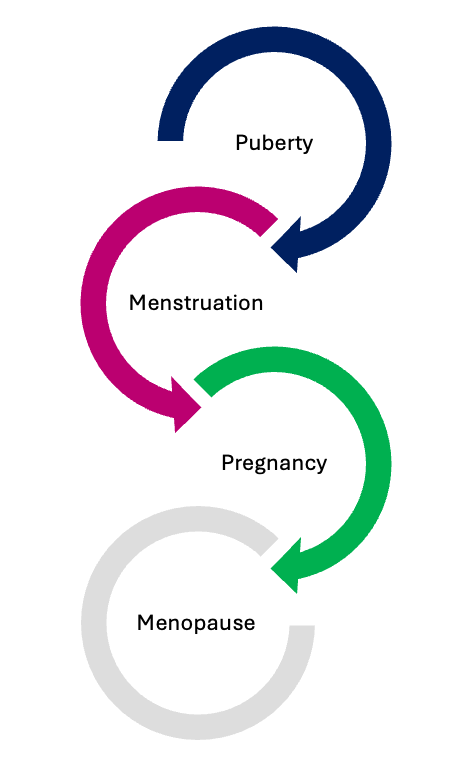
There are differences between the general health needs of a man and a woman, and hormonal fluctuations have a strong influence on systemic and oral health, especially through different stages in a woman’s life.
Before the latest S3 guidelines, we used to classify some periodontal conditions according to the onset of puberty and pregnancy-related conditions, so we already accepted the link between hormonal imbalance and oral diseases.
During menstruation, hormonal changes make patients sensitive or prone to gingival inflammation. This moves through to pregnancy where many women suffer from pregnancy gingivitis, or their already diagnosed periodontitis deteriorates.
Then the last stage is menopause where women spend about a third of their life, and at this point, well, we don’t know much about it and it’s an awkward subject, so we just leave it alone.
Menopause and the life cycle
Before the latest S3 guidelines, we used to classify some periodontal conditions according to the onset of puberty and pregnancy-related conditions, so we already accepted the link between hormonal imbalance and oral diseases.
During menstruation, hormonal changes make patients sensitive or prone to gingival inflammation. This moves through to pregnancy where many women suffer from pregnancy gingivitis, or their already diagnosed periodontitis deteriorates.
Then the last stage is menopause where women spend about a third of their life, and at this point, well, we don’t know much about it and it’s an awkward subject, so we just leave it alone.
Menopause causes biological and endocrine changes, particularly sex steroid hormones. Hormones are classified due to their chemical structure and there are over 50 different types. They control functions of body systems and organs, and control growth and development.
Hormones are chemical messengers released by the endocrine gland into the bloodstream. A collection of hormonal changes occurs before, during and after menopause, with the main sex steroid hormones being estrogen alongside some alteration in progesterone and testosterone.
Hormones are packaged, synthesised, and immediately released for use, so not stored in cells. Oestrogen is the main group of hormones which is sub-divided into:
- Estradiol
- Estriol
- Estrone.
They all have functions at different stages in the life cycle and help to protect the heart, our mood and bone strength.
What is the menopause?
- Menopause is a normal developmental stage when the ovaries stop producing eggs and menstruation permanently ceases
- Irreversible changes in the hormones and reproductive systems of the ovaries
- Declining levels of oestrogen and other hormones (progesterone and testosterone)
- The average age in the UK is 51 years
- Defined as a year after the last period
- Early menopause can occur before 45 but for no apparent reason.
Menopause is a permanent reduction of oestrogen, progesterone and often testosterone. It brings on a wide range of symptoms and an increased risk of inflammatory conditions such as heart disease, osteoporosis and dementia
Menopause symptoms – it’s not just hot flushes!
Women have oestrogen receptors on every cell in their bodies. This means that without oestrogen, many different symptoms can occur.
Some women experience very few symptoms whereas others experience several of them. In addition, symptoms can vary with time, with some symptoms improving and then others developing. There are over fifty different symptoms, and they can be physical, psychological or vasomotor (related to heat regulation).
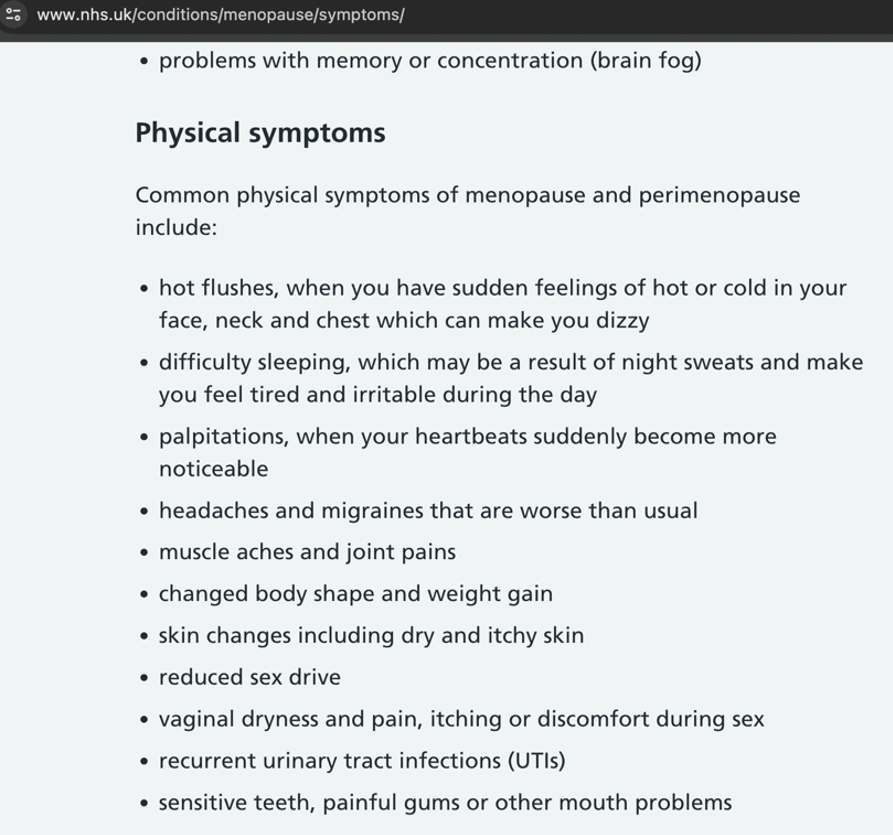
Regarding the oral cavity, it can be seen from the NHS conditions online that teeth and gums are listed as physical symptoms.
Delta Dental in America conducted a study where they surveyed 1,000 women with menopausal symptoms and found that 84% were not aware of the impact of oral health changes and menopause. In addition, 79% had noticed some degree of change with their teeth or gums but not reported it to their dental professional.
The three stages of menopause
Oestrogen is the most abundant hormone in females. It powers the menstrual cycle and provides female characteristics – the ovaries make most of the oestrogen, as well as the adrenal glands and fat tissues.
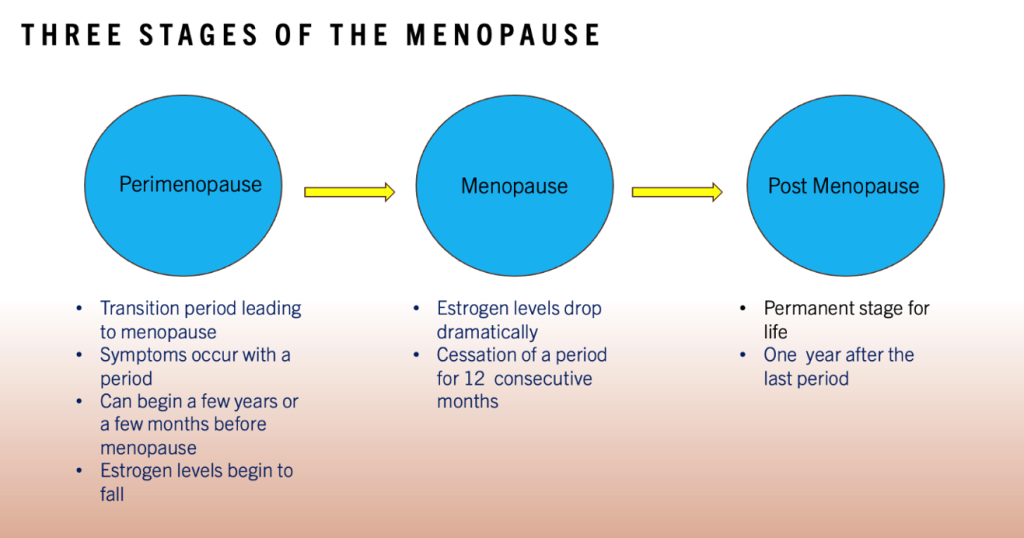
The relationship between oral discomfort and menopause was investigated by Waldrop et al in 1989. It was a comparative study of 149 women split into three groups. Group one was perimenopausal, group two was menopausal women undergoing no treatment and group three was menopausal attending a menopause clinic or starting treatment (having a series of tests and blood tests).
In group three, the oral discomfort was reported in 33% of women, as well as 43% of those in the perimenopause phase. Two thirds of women found their oral discomfort without clinical signs.
Oro-dental conditions
We can broadly categorise oral manifestations that can occur into three subgroups as discussed and investigated by Chander et al. Xerostomia and burning tongue syndrome appear to be the more commonly reported symptoms.
Salivary function
Saliva plays a key role in the oral defense mechanism. It has many functions including mastication, lubrication, swallowing and plaque neutralisation. Medications are often the number one reason for reduced salivary function, so this should be considered.
Oestrogen receptors are present in the oral mucosa, and both salivary glands and diminishing levels of oestrogen can contribute to changes in salivary levels.
Xerostomia (dry mouth) is a reported condition associated with a reduction in salivary flow giving the sensation of oral dryness, usually with hypo-salivation but not always. It creates marked discomfort in patients with removable dentures and cracked lips.
Fluctuations in salivary flow have been explored with some studies showing the composition of saliva changing amongst peri and post-menopausal women being oestrogen-dependent. However, some studies show no change or correlation.
Alterations to saliva components, such as the lysozyme enzyme (part of saliva and found in gingival circler fluid), were investigated by Rukmani et al as part of a cross-sectional study in Bengaluru.
A reduction in saliva flow can increase the incidence of caries and oral candidiasis as well as an increase in plaque biofilm on the tooth surface. In turn, this can initiate or deteriorate gingivitis and periodontal disease status.
Oral mucosa
The oral mucosal contains oestrogen receptors and variations in hormone levels which directly affect the oral cavity. When looking histologically, the oral mucosa resembles the vaginal mucosa so the response to diminishing oestrogen levels is similar.
Mucosal atrophy can occur as oestrogen affects the oral mucosal epithelium, causing thinning and making it more susceptible to injury, trauma and increased risk of inflammation.
Oral candidiasis (oral thrush) is a fungal infection caused by the overgrowth of candida albicans. The onset of menopause can cause the overgrowth to become more rapid.
Burning mouth syndrome (BMS) or glossdynia is a common symptom reported, but other systemic causes or conditions should be addressed before the possibility of it being related to menopause. It is described as a burning sensation which is normally bilateral but frequently involving the anterior two-thirds of the tongue, the dorsum, and lateral borders of the mucosa and the lower lip. In addition, it often involves more than one site but with no apparent clinical change. It can also involve loss of taste being reported in peri-menopausal women.
Teeth and periodontium
The decrease in oestrogen levels can lead to changes in the gum tissues, making them more susceptible to inflammation and infection.
With periodontitis, changes to bone resorption can cause accelerated bone loss deteriorating the periodontal status with systemic inflammation leading to chronic inflammation.
There is a higher risk of osteoporosis with a reduction in bone loss density, which can increase the risk of developing osteoporosis. When bone density compromises the jaw, the risk of tooth loss is greater, especially if a woman has periodontal disease. In some cases, it can accelerate the progression of periodontal disease and these patients will need careful periodontal assessment and reviewing and referrals.
The breakdown of bone resorption and formation process has a particular focus on resorption. Bone-forming osteoblasts and bone-resorbing osteoclasts contain oestrogen receptors. Osteoporosis is a silent disease with no pain, and it is only when bone fractures occur that pain is felt. Regarding the oral cavity, this can lead to tooth loss as the bony framework providing anchorage for the teeth is compromised.
Dental caries (especially root caries) are at risk of increasing during the menopause phases due to a combination of factors like low saliva, elevated plaque levels and root caries more commonly associated with the older population. Other lesser-reported symptoms can occur like lichen planus.
As a dental professional, how can you help?
You are all probably already assessing your patients and treating them accordingly. The list below provides a summary:
- Comprehensive examination
- Detailed clinical/social history
- Periodontal assessment
- Salivary assessment if required
- Tailored oral hygiene
- Professional mechanical plaque removal (PMPR).
In addition:
- Salivary substitutes
- Smoking cessation
- Low/moderate alcohol
- Good diet
- Low sugary/ acidic foods and drinks
- Avoid spicy food
- Drink plenty of water.
- The Balance App can help monitor menopausal symptoms.
Products such as Oralieve Moisturising mouth gel can help with dry mouth, Gengigel for burning mouth symptoms, as well as Biomin F toothpaste to combat root caries and sensitivity.
Hormone replacement therapy
Hormone replacement therapy (HRT) replaces or tops up hormones the body no longer produces or is not making enough off. It can help to reduce menopausal symptoms with a medicine that has oestrogen, or oestrogen and progesterone combined.
HRT may also help prevent osteoporosis in some people, but it is recommended as a balance of risk and benefit, as it has been reported to possibly increase the risk for other health conditions, including heart disease, breast cancer, blood clots in the legs or lungs and stroke.
It has been recently reported that only 5% of women worldwide take HRT and 14% of women in the UK.
In conclusion, oestrogen receptors are found in the oral cavity and salivary glands, and women transitioning through the stages of menopause do report oral discomfort.
However, there are not enough longitudinal studies to statistically state a direct correlation between menopause and oral symptoms.
I would like this article to encourage you all to be bold and brave in approaching the subject of menopause with women who may be going through this natural development stage.
Contact [email protected] for references.
Follow Dentistry.co.uk on Instagram to keep up with all the latest dental news and trends.


