
Charlotte Leigh discusses the dangers of undiagnosed obstructive sleep apnoea, and why dentists are uniquely placed to screen and treat it.
If you could save your patients’ lives, you would, wouldn’t you?
I am Charlotte Leigh and I graduated from the University of Leeds 2012 and work in general practice at Montagu Dental. I completed my MSc in restorative dental practice with distinction at the Eastman Dental Institute in 2019. During my final year, I wrote my dissertation on ‘What do GDPs know about Snoring and Obstructive Sleep Apnoea?‘ The answer is very little, and this inspired my journey.
We are in a privileged position as dentists to help our patients improve their quality of life. Helping patients treat their snoring or screening a patient for obstructive sleep apnoea can not only improve the sleep quality for the patient and their families, but salvage marriages and save a life.
Technological distractions, work pressures, the ‘sleep is for wimps’ culture, and the maxim ‘I’ll sleep when I’m dead’ has led to the association of this natural, fundamental and critical bodily function with laziness. The full cost of sleep deprivation to the health service is not well reported, but likely to have high financial implications and cause a huge societal burden.
Sleep provides the body with the opportunity to restore the immune, nervous, skeletal, and muscular systems nightly, which is crucial to maintain mood, memory, and cognitive function.
What is obstructive sleep apnoea?
Snoring is part of sleep-related breathing disorders that can be regarded as being on a spectrum with simple snoring at one end and obstructive sleep apnoea (OSA) at the other. This is when there is partial or total obstruction of the upper airways during sleep.
OSA is often poorly recognised and under diagnosed, yet it’s common, affecting an estimated 1.5 million adults in the UK. Up to 85% of this total are undiagnosed and therefore untreated.
OSA occurs when the airway is partially or totally obstructed during sleep. The partial obstructions (hyponeas) or total obstructions (apnoeas) often result in loud noises, oxygen desaturation, and patients often wake up gasping for breath.
Symptoms may include daytime sleepiness, loud snoring, dry mouth and restless sleep. Undiagnosed and untreated OSA can lead to multiple health conditions including cardiovascular disease, hypertension, heart disease, stroke depression and daytime sleepiness.
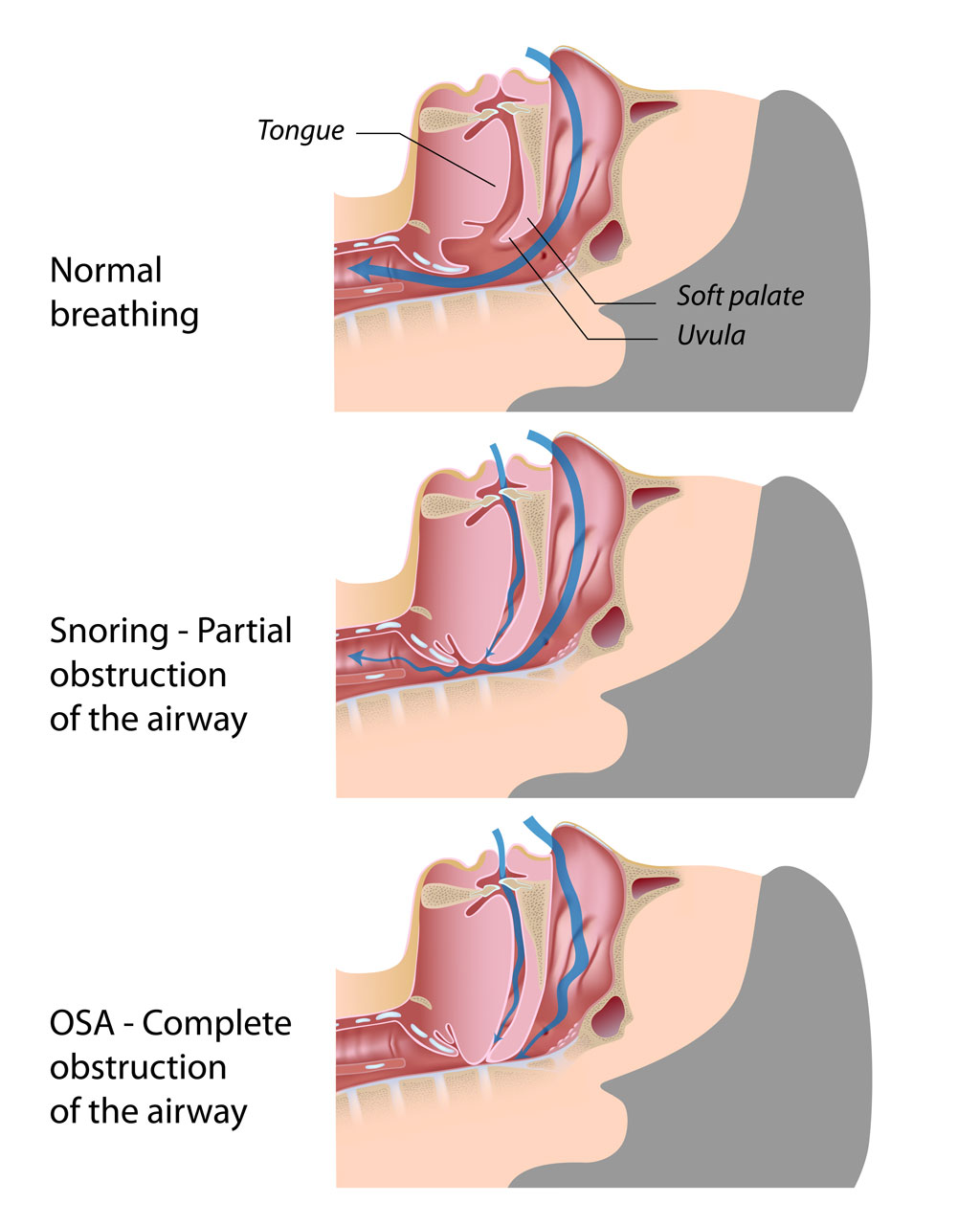
Snoring is the hoarse or harsh sound that occurs when air flows past relaxed tissues in your throat, causing the tissues to vibrate as you breathe. Most people snore at some point during their sleep cycle, but for some it can be a chronic problem.
The risks of obstructive sleep apnoea
Snoring can create loud noises, which disturb sleep for the whole family. Some patients have been reported as snoring louder than a jet plane! Poor quality sleep affects productivity, efficiency, decision making, nutrition choices and often leads to more chronic health conditions.
There are certain characteristics that increase the risk of snoring, including anything that increases the risk of upper airway infection or inflammation. Nasal obstruction, smoking or alcohol dependence, being male and individual’s body mass index (BMI) and neck circumference (17+ inches) is strongly correlated to sleep related breathing disorders.
Snoring itself is not thought to pose a risk to the health as such, but as part of the continuum there is a risk of it developing into OSA, and this alone merits early treatment.
Diagnosing and treating obstructive sleep apnoea
Screening is often conducted easily in surgery with questionnaires and a dental examination. Home sleep tests can be used to highlight oxygen desaturation and measure many apneas or hypopneas occurring during a patients sleep.
As dentists, we are uniquely placed to assist in the screening process including assessing upper airway tissue and contributing craniofacial morphology. There are also strong correlations between patients who suffer with bruxism and gastro-oesphageal reflux disorder.
I would encourage dentists to screen their patients who suffer from bruxism for obstructive sleep apnoea, as the appliance that you recommend may actually make their snoring worse.
Treatment for snoring and OSA depends on the cause. Simple lifestyle measures include weight loss (if necessary), reduction in alcohol, ceasing smoking, optimal nutrition and good sleep hygiene are often first line measures. Other recommendations can include myofunctional exercises, mandibular advancement devices, continuous positive airway pressure (CPAP) and surgery.
The newly evolved specialism of sleep medicine is rapidly gaining popularity due to an increased awareness about the consequences of lack of sleep. Dentists are uniquely placed to screen and treat these patients with mandibular advancement devices and should be included in the sleep management team.
The National Institute for Health and Care Excellence (NICE) guidelines published in 2021 discusses use the of mandibular advancement devices as a treatment option.


