 Rachel Derby and Enikő Sztuparity discuss restoring congenitally absent lateral incisors in teenagers from the perspective of dentist and technician.
Rachel Derby and Enikő Sztuparity discuss restoring congenitally absent lateral incisors in teenagers from the perspective of dentist and technician.
Restoring congenitally absent lateral incisors in teenagers can be clinically challenging.
As a clinician, you must try and look to the future and plan for further restorations and implants for when your restorative work eventually fails.
You must also be able to communicate this ongoing restorative cycle to the patient and, more importantly, their parents.
Case study
Patient ZG, a 15-year-old male, attended the clinic with his mother looking for restorative solutions for his UR2 after having his fixed braces deboned.
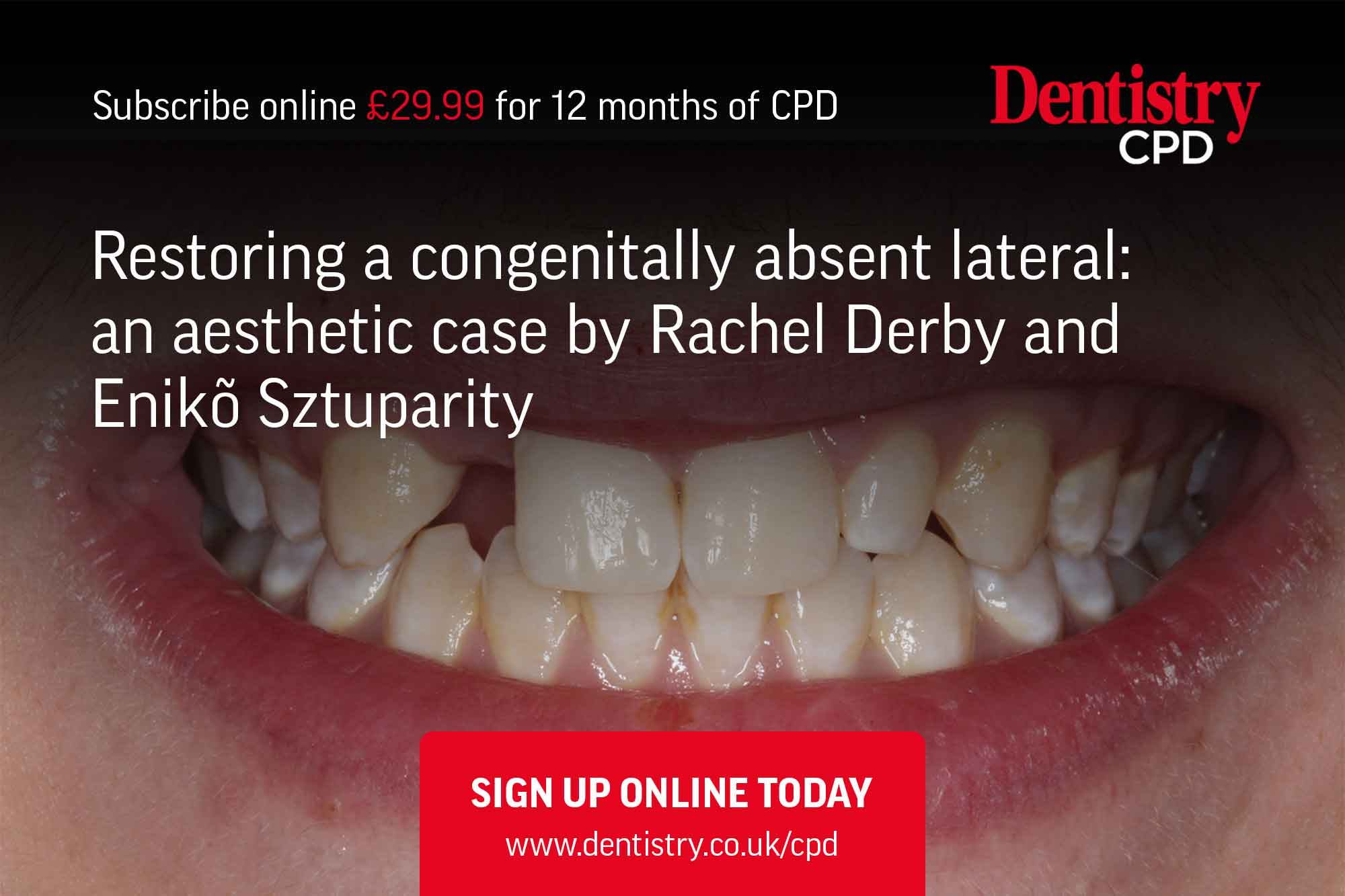
Examination showed that the patient had a congenitally missing UR2 and a diminutive UL2. His oral hygiene was good and there was mild to moderate levels of fluorosis on his teeth.
Orthodontic treatment had left the patient in a class one incisal, molar and canine relationship. It had provided 6mm of space in which to place a restoration.
The patient was currently wearing an Essex retainer with a pontic in the UR2 area, but hated taking it out at school to eat.
A full series of clinical photography was used to help plan this case (Figures 1 to 5).
Treatment planning process
The ideal treatment to replace the UR2 would be an implant.
On average, an implant has a survival rate of 94.6% over 13.4 years (Moraschini et al, 2015). However, in this case, the patient was too young. If we were to place an implant now, the implant would act as an ankylosed tooth, it would be fixed in place.
Jaw growth would still occur until adulthood, which for a male would be approximately 24 years, perhaps longer. This would result in the teeth moving, but the implant crown would be fixed in its original place, resulting in an unaesthetic look.
We needed a solution for the medium- to long-term until a time an implant would be suitable.
If we leave the space and do nothing, the teeth will move and we will lose the space.
A single tooth denture was a possibility, however, the patient and mother declined this option. Socially, the patient did not want a denture, or to be known amongst his peers as having a denture.
A bridge would be the only viable option for this patient. A conventional bridge would be extremely destructive, but a resin retained cantilever bridge (RRB) would work well.
A study completed at Bristol University in 2015 by King and colleagues indicated that RRB with minimal tooth preparation had superior longevity than those with other preparation designs.
The study also showed that the survival of a resin retained bridge at five years was 80.8% and 80.4% at 10 years (King et al, 2015).
A resin retained bridge would be the best fixed option for patient ZG and, if we get it right, it will last until he is ready for an implant.
It would be best to place the wing of the RRB onto a canine tooth, this is due to the greater surface area that it provides. In addition, the aesthetics are not as affected as the metal of the wing tends not to shine through and darken the tooth.
However, in the case of ZG, the canine was small and would not provide as great a surface area compared to his central incisor. If we place the metal wing on the central incisor, the metal can shine through.
Research is now showing that bonded zirconia-based resin retained bridges can provide excellent outcomes as they:
- Are highly durable
- Are aesthetic
- Have a high survival and success rate. One study demonstrated a 10-year survival rate of 98.2% and a success rate of 92% (Kern et al, 2017).
What about the UL2? By placing a RRB in the UR2, we would be restoring it to ideal height and width. If we left the UL2 alone, the symmetry would be off. A veneer could be placed to match the height and width, however, no matter how minimal we try to be, this would require irreversible tooth preparation.
A composite veneer would require no preparation and provide a cosmetic result. If the patient decided to have a veneer when he was older then he would still be able to.
The treatment plan was a zirconia-based resin retained bridge using the UR1 as an abutment to replace the UR2 and a composite veneer to restore the UL2.
To read the rest of this article and gain CPD for it, simply visit www.dentistry.co.uk/cpd.


