 Neil Patel discusses the first part of a clinical case where he closes the anterior open bite of a young patient.
Neil Patel discusses the first part of a clinical case where he closes the anterior open bite of a young patient.
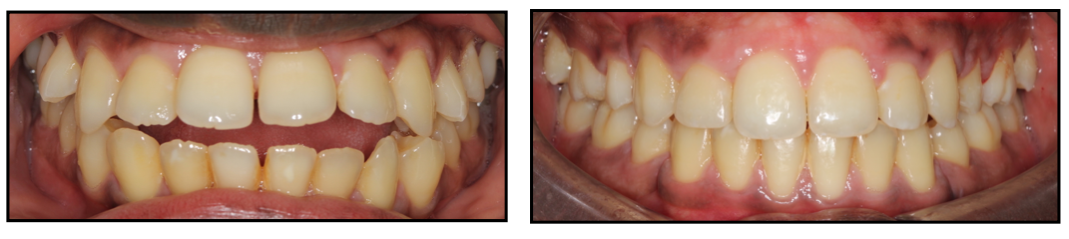
Patient overview
- Male patient, age: 24
- Treated with extraction of all four first premolars teeth
- Upper and lower fixed appliances
- Upper and lower fixed and removable retention.
An anterior open bite (AOB) can be defined by a gap between the anterior teeth (incisors), that is, by a deficiency in the normal vertical overlap between antagonist incisal edges when the posterior teeth are in occlusion.
An AOB can exist for several reasons. Only once the aetiology is diagnosed can the treating clinician offer the correct treatment plan.
Dentistry’s top stories
Anterior over bite causes
Common causes of an AOB you can find on the list below and we can divide into dental, soft tissue and skeletal.
Dental causes:
- Thumb sucking
- Abnormal eruption from ankylosis
- Over-eruption of molar teeth
- Tooth wear without secondary or compensatory eruption.
Soft tissue:
- Forward tongue thrust.
Skeletal:
- An increased mandibular plane angle with an increase in the lower vertical facial height.
Patient history and examination
This patient was concerned about:
- Large gap between the front teeth leading to difficulty eating and drinking
- Unhappy with the aesthetic appearance of his smile
- Forward protrusion of his front teeth.
He presented with a class III incisor relationship on a class III skeletal base, increased vertical facial heights and no significant transverse discrepancy.
The main features of his oral health and malocclusion included:
- Periodontal disease BPE 111/121
- Mild crowding in the upper arch and lower arch
- Mild spacing in the upper and lower arch
- Bimaxillary proclination
- 1/4 unit Class III buccal segments
- Active tongue thrust.
Medical history – nil.
Social history – non smoker.
Dental history – regular attendee, electric toothbrush twice daily, irregular use of dental floss and interdental brushes. Thick gingival biotype.
*The patient previously had an orthodontic consultation three years ago. Subsequently he was referred to a secondary care unit for a joint orthodontic and orthognathic appointment, where an orthodontic and surgical treatment plan was offered.
The patient declined a surgical treatment plan and sought an orthodontic camouflage option.
Diagnosis and treatment plan
In this case we diagnosed that the aetiology of the AOB was:
- Soft tissue – forward tongue posture
- Dental – proclined upper and lower labial segments
- Skeletal – increased lower vertical facial height.
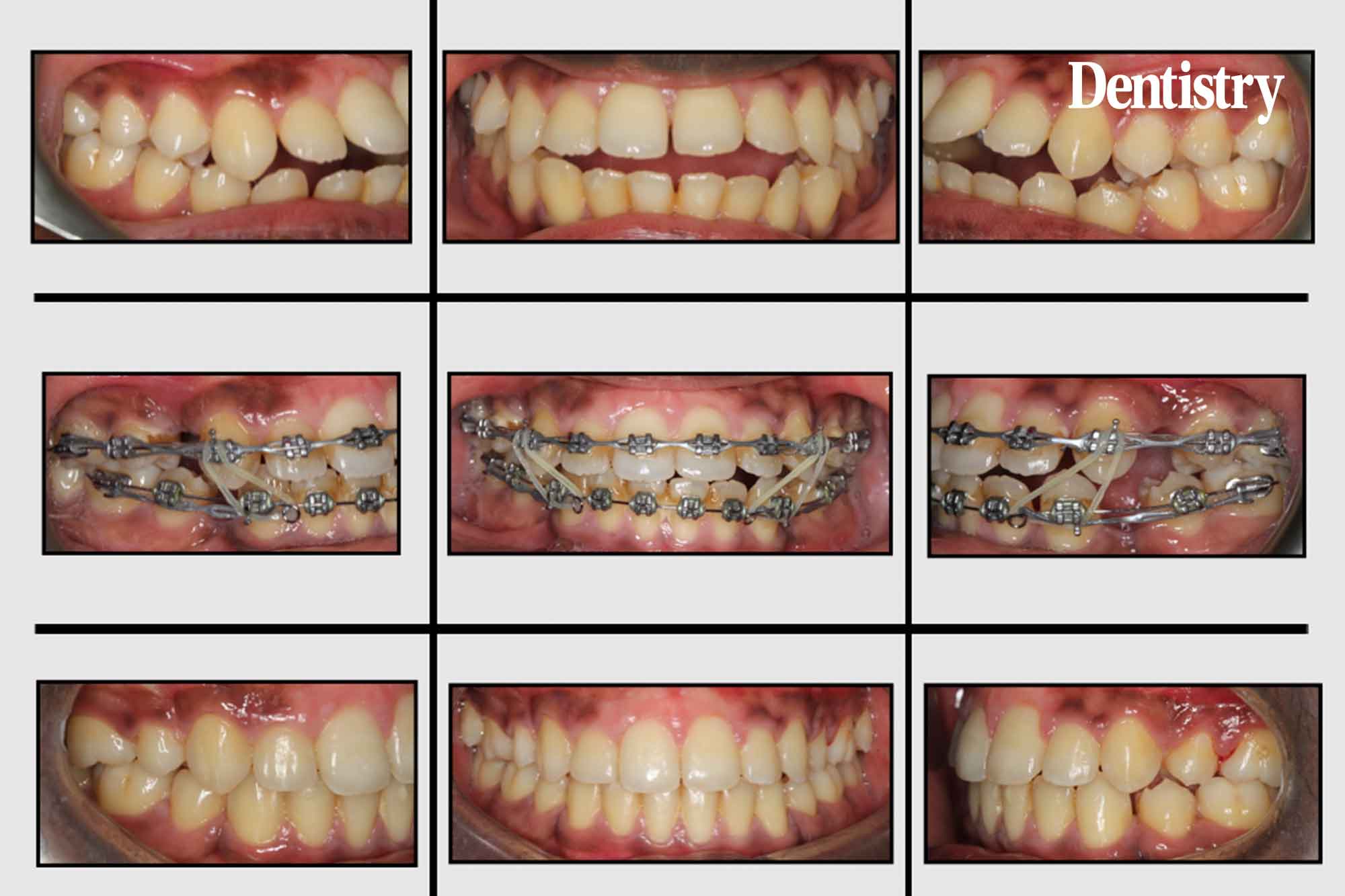
Taking the clinical examination and cephalometric analysis into account it was deemed this case was suitable for orthodontic camouflage treatment in order to achieve an optimal clinical result.
Treatment plan
- Extraction of the UR4 UL4 LR4 LL4 (upper and lower right and left first premolar teeth)
- Upper and lower fixed appliances
- Tie backs from all canines to all first permanent molars – this is done to protect the archwires in the early stages and aid canine retraction
- Anterior box elastics to aid AOB closure
- Upper and lower fixed retainers and upper and lower thermoplastic retainers, long term.
Treatment objectives
- Align and level upper and lower arches
- Correct mild lower centreline discrepancy
- Retrocline upper and lower labial segment and in doing so:
-
- Correct AOB to an average overbite
- Space closure – mesial movement of the buccal segments and distalisation of the labial segments
- Incisor relationship correction to class I
- Correct bimaxillary proclination and improve the inclination of the upper and lower labial segments.
Case based discussion
Anterior open bites are extremely difficult to treat with orthodontics alone. And there is a high risk of relapse if the movements planned are unstable.
In this particular case the key features, which allow orthodontics alone to correct the moderate AOB, were:
- The patient presented with bimaxillary proclination
- Thick gingival biotype
- Excellent patient compliance with anterior and posterior elastic wear.
Why extract teeth?
Although there appears no obvious crowding from the pre-treatment clinical photography, there is a relatively steep lower curve of spee (vertical crowding). Once levelled this would procline the upper and lower labial segments further.
Extraction space is therefore required to level the curve of spee, as well as retrocline the labial segments to correct the AOB.
The importance of retention
We instructed the patient, following debond, of the fixed appliances. As well as the importance of seeing their dental hygienist the same day, due to build up of lingual calculus during treatment.
Two days later we fitted upper and lower fixed bonded retainers.
It was empahsised to the patient that placement of the bonded retainers and regular night time wear of the thermoplastic retainers was paramount in order to counteract:
- Relapse from extrusive movements during treatment
- His active tongue thrust.
In addition to the maintenance of a good overbite with favourable skeletal changes, the correction of an AOB is also attributed to correct diagnosis, sound orthodontic treatment planning and correct use of mechanics.
Soft tissue factors such as an active tongue thrust is out of the clinicians control. We must discuss this in detail with the patient with regards to long-term stability.

Catch previous Ortho expert columns
- Invisalign case study part three: periodontal drifting and a class III malocclusion
- Invisalign case study part two: mild class III and reduced overbite
- Invisalign case study part one: the deep bite
- How to master the virtual consultation.
Follow Neil on Instagram, @neilortho, and ask the ortho expert questions anything orthodontic related.
Follow Dentistry.co.uk on Instagram to keep up with all the latest dental news and trends


