Dental hygienist Janet Williams Oshun investigates how oral health is influenced by culture and varying oral practices.
In the final year of my studies at the Dublin Dental University Hospital, I conducted research to uncover the impact of ethnic and cultural oral practices with the aim of highlighting the need to incorporate culturally inclusive approaches to oral care.
Oral health is not just a matter of brushing and flossing. It’s deeply intertwined with individual lifestyles factors, our social and community networks, living and working conditions and general socio-economic, cultural and environmental conditions. My research centres on the intricate relationship between culture and oral health. I believe that this area is underrepresented in the dental industry.
This article focuses on three widely used oral health practices: the miswak, betel nut chewing, and oil pulling therapy.
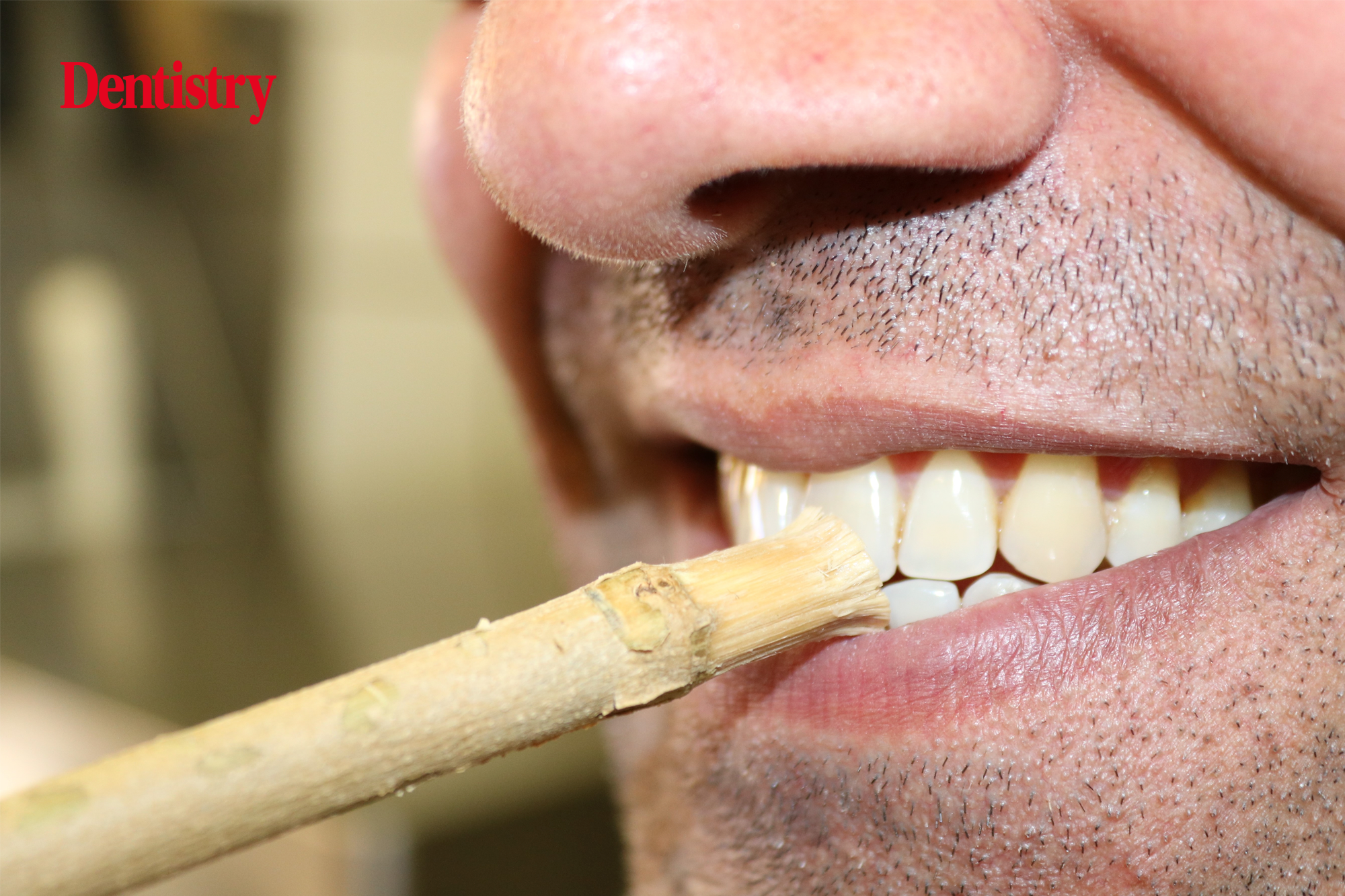
The miswak: a sacred ritual for oral health
Firstly, let’s delve into the remarkable world of the miswak. The miswak is essentially a natural toothbrush made from a twig taken from the Salvadora persica, or Arak tree. It is still commonly used in the Middle East, North Africa and Central and Southeast Asia and is seen as a sacred ritual for the spiritual purification of the mouth and mind (Saha et al, 2012). The World Health Organization (WHO) recognises this spiritual view and has stated that miswak use is not only inexpensive, but also an effective tool for oral hygiene (Aboul-Enein, 2014).
The secret to the miswak’s extraordinary oral health benefits lies in its composition. The miswak releases natural bioactive chemicals, such as calcium, fluoride, benzyl isothiocyanate, vitamin C, tannic acid and more when chewed, offering a myriad of benefits.
Miswak reduces plaque and gingivitis, aids enamel remineralisation, prevents carcinogenic and genotoxic compounds and promotes healing and tissue repair (Haque and Alsareii, 2015). An evidence-based review (Nordin et al, 2020) confirms its antifungal, anticariogenic, antibacterial, and antiplaque effects.
Yet, for all its virtues, the miswak is not without disadvantages. The miswak’s structure limits access to interdental spaces, lingual and palatal surfaces (Gazi et al, 1990), and some studies have shown that it can cause occlusal wear and gingival recession (Johansson et al, 1991; Eid and Selim, 1994).
The literature showcases the importance of advocating for its use, with the requirement that it should be accompanied by auxiliary oral hygiene aids like interdental brushes and dental floss.
Betel nut chewing: a cultural tradition with dental consequences
Next, we’ll turn our attention to betel nut chewing. This cultural ritual is deeply rooted in the cultures of South and Southeast Asia, the Pacific Islands, and parts of Africa. It involves chewing the betel nut (areca nut) without swallowing it. It is often combined with a blend of tobacco, spices, and betel nut leaves to create a ‘betel quid’.
An estimated 600 million people worldwide consume betel nut and betel quid (Gupta and Warnakulasuriya, 2002). Remarkably, it ranks as the fourth most consumed psychoactive substance globally, following nicotine, caffeine, and alcohol. It induces effects like euphoria, energy boost, satiation, and relief from toothaches (Anand et al, 2014).
From an oral health perspective, betel nut chewing brings various risks to both hard and soft oral tissues, leading to root and tooth fractures, occlusal tooth loss, and the potential of temporomandibular joint degeneration in chronic users. However, some suggest it may offer protection against caries (Trivedy et al, 2002).
Furthermore, betel nut chewing elevates the risk of periodontal disease, oral cancers, and oral submucosal fibrosis (Anand et al, 2014). The WHO has classified betel nut as a group one human carcinogen (WHO, 2012). It contributes to cancer initiation through genotoxicity and gene mutation (Anand et al, 2014).
This cultural practice has been shown to have detrimental effects on the oral cavity. Due to limited evidence of positive impact, it calls for discouragement in oral care.
Oil pulling therapy: an ancient practice with modern potential
Lastly, we will explore oil pulling therapy, firmly established in Ayurvedic (Hindu) culture in India. This age-old practice involves swirling one tablespoon of oil in the mouth for 10 to 20 minutes on an empty stomach and then spitting it out (Hariharan et al, 2020).
It is rooted in the belief that this process removes impurities from the body through the tongue and saliva and increases good oral health (Singh and Purohit, 2011).
Oil pulling is known for its antioxidant and antibacterial properties, and reduces plaque, gingivitis and halitosis. It may even have potential curative effects on systemic diseases like migraines, diabetes, and asthma (Asokan et al, 2009).
The antioxidants in oil pulling target and eliminate pathogenic bacteria, such as A actinomycetemcomitans and P gingivalis (Sood, 2014). Studies indicate that sesame oil, a common choice, can be as effective as chlorhexidine in preventing plaque-induced gingivitis (Shanbhag, 2017) and combating oral malodor and pathogenic bacteria (Sood, 2014).
Although it’s not advised for children under five years due to the risk of aspiration (Hariharan et al, 2020) and time-consuming nature (Sood, 2014), oil pulling offers notable benefits.
Many studies have shown significant positive results for oil pulling. However, my research found most studies were only over a short period of time (two weeks to a month). More research into the long-term effects and its place within western culture would be beneficial.
Awareness of culture in oral health care
As dental health professionals, our foremost responsibility is to act in the best interest of our patients. Fostering cultural inclusivity is central to this mission.
To accomplish this, it is essential to gain a profound understanding of diverse oral practices from around the world. Applying this knowledge in the delivery of oral health instructions, dietary advice, treatment plans and more encourages openness and receptiveness to our guidance.
This journey is about enriching our comprehension of our patients’ culture and customs. By embracing culture and diversity in oral healthcare, we can significantly improve the quality of care we provide for patients.
References
- Aboul-Enein, B.H. (2014). The miswak (Salvadora persica L.) chewing stick: Cultural implications in oral health promotion. The Saudi Journal for Dental Research, 5(1), pp.9–13. doi:https://doi.org/10.1016/j.ksujds.2013.06.002.
- Anand, R., Dhingra, C., Prasad, S. and Menon, I. (2014). Betel nut chewing and its deleterious effects on oral cavity. Journal of Cancer Research and Therapeutics, 10(3). doi:https://doi.org/10.4103/0973-1482.137958.
- Asokan, S., Emmadi, P. and Chamundeswari, R. (2009). Effect of oil pulling on plaque induced gingivitis: A randomized, controlled, triple-blind study. Indian Journal of Dental Research, 20(1), p.47. doi:https://doi.org/10.4103/0970-9290.49067.
- Eid, M.A. and Selim, H.A. (1994). A retrospective study on the relationship between miswak chewing stick and periodontal health. Egyptian Dental Journal, [online] 40(1), pp.589–592. Available at: https://pubmed.ncbi.nlm.nih.gov/9588141/ [Accessed 20 Mar. 2023].
- Gazi, M., Saini, T., Ashri, N. and Lambourne, A. (1990). Meswak chewing stick versus conventional toothbrush as an oral hygiene aid. Clinical preventive dentistry, [online] 12(4), pp.19–23. Available at: https://europepmc.org/article/med/2088630 [Accessed 12 Apr. 2023].
- Gupta, P.C. and Warnakulasuriya, S. (2002). Global epidemiology of areca nut usage. Addiction Biology, 7(1), pp.77–83. doi:https://doi.org/10.1080/13556210020091437.
- Haque, M. and Alsareii, S. (2015). A review of the therapeutic effects of using miswak (Salvadora persica) on oral health. Saudi Medical Journal, 36(5), pp.530–543. doi:https://doi.org/10.15537/smj.2015.5.10785.
- Hariharan, R., Aravindha Babu, N., Masthan, K. and Rajesh, E. (2020). Oil pulling and its oral benefits – a review. European Journal of Molecular & Clinical Medicine, 07(03), pp.1792–1797.
- Johansson, A., Fareed, K. and Omar, R. (1991). Analysis of possible factors influencing the occurrence of occlusal tooth wear in a young Saudi population. Acta Odontologica Scandinavica, [online] 49(3), pp.139–145. doi:https://doi.org/10.3109/00016359109005898.
- Nordin, A., Bin Saim, A., Ramli, R., Abdul Hamid, A., Mohd Nasri, N.W. and Bt Hj Idrus, R. (2020). Miswak and oral health: An evidence-based review. Saudi Journal of Biological Sciences, 27(7), pp.1801–1810. doi:https://doi.org/10.1016/j.sjbs.2020.05.020.
- Saha, S., Mohammad, S., Saha, S. and Samadi, F. (2012). Efficiency of traditional chewing stick (miswak) as an oral hygiene aid among Muslim school children in Lucknow: A cross-sectional study. Journal of Oral Biology and Craniofacial Research, 2(3), pp.176–180. doi:https://doi.org/10.1016/j.jobcr.2012.10.009.
- Shanbhag, V.K.L. (2017). Oil pulling for maintaining oral hygiene – A review. Journal of Traditional and Complementary Medicine, [online] 7(1), pp.106–109. doi:https://doi.org/10.1016/j.jtcme.2016.05.004.
- Singh, A. and Purohit, B. (2011). Tooth brushing, oil pulling and tissue regeneration: A review of holistic approaches to oral health. Journal of Ayurveda and Integrative Medicine, 2(2), p.64. doi:https://doi.org/10.4103/0975-9476.82525.
- Sood, P. (2014). Comparative Efficacy of Oil Pulling and Chlorhexidine on Oral Malodor: A Randomized Controlled Trial. Journal of Clinical and Diagnostic Research. doi:https://doi.org/10.7860/jcdr/2014/9393.5112.
- Trivedy, C.R., Craig, G. and Warnakulasuriya, S. (2002). The oral health consequences of chewing areca nut. Addiction Biology, 7(1), pp.115–125. doi:https://doi.org/10.1080/13556210120091482.
- World Health Organization, 2012. Review of areca (betel) nut and tobacco use in the Pacific: a technical report.
Janet’s NSK Ikigai webinar can be watched on demand at mynsk.co.uk/ikigai/webinars/.
This article is copyright of Janet Williams Oshun and appears with permission.


