 Stephen Hancocks explains the process behind manufacturing the perfect syringe with local anaesthetic to deliver to your patients.
Stephen Hancocks explains the process behind manufacturing the perfect syringe with local anaesthetic to deliver to your patients.
How many times a day do we pick up a syringe with a local anaesthetic cartridge in it? Probably dozens, but how many times do we pause and ponder the complexities of the processes in getting it to us?
We need to be aware, of course, of the components of a local anaesthetic cartridge for appropriate patient safety and of the expiry date. But beyond that our knowledge of the processes behind the chemistry and manufacture are probably limited.
Firstly, the contents need sterilising and there are two possible processes to ensure this; either aseptic manufacturing or terminal sterilisation.
For each particular drug product, it is the manufacturer’s responsibility to undertake the appropriate investigations to determine which is the most suitable of process and to then submit the results for assessment and approval by the relevant authorities.
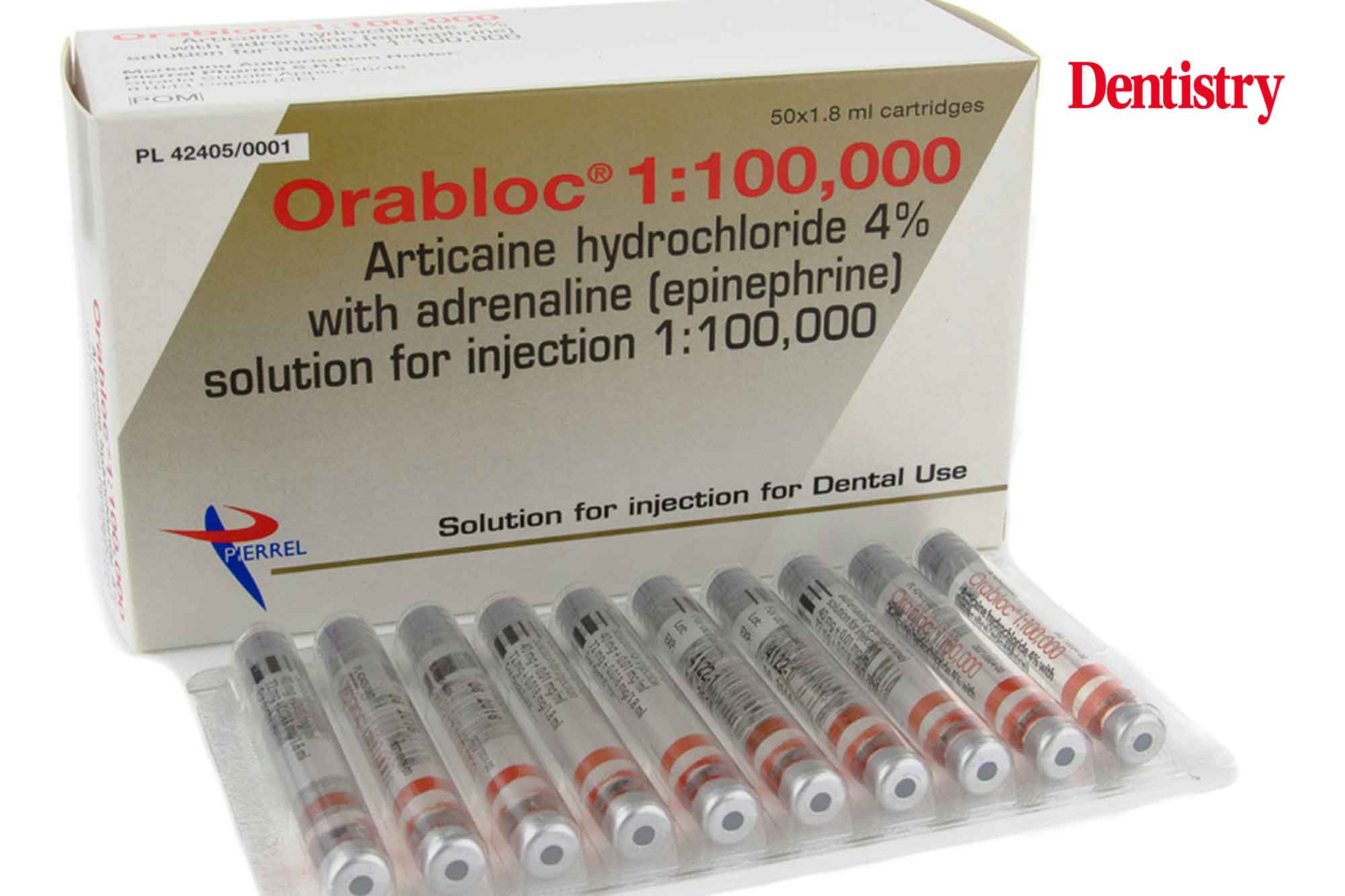
As most of us are aware, the majority of dental anaesthetics contain a vaso-constrictor such as ‘epinephrine’ (adrenaline); for example Orabloc (articaine hydrochloridre 4% and epinephrine). The characteristics and chemistry of which are well documented in the literature.
However, it is a reducing substance and as such is easily oxidised. As a consequence it requires protection by a suitable anti-oxidant. This is usually in the form of a sulphite or metabisulphite.
A further consideration involves the primary container closures of a rubber plunger and rubber cap seal. Necessarily, the characteristics of the rubber need researching during the development steps of the drug product to establish any potential extractables and leachables. Plus the stability of the rubber characteristics at a range of temperatures.
Establishing the perfect manufacturing process
Several steps need evaluating in order to decide which of the two manufacturing processes is better for dental anaesthetics containing epinephrine:
- The chemical, physical and microbial characteristics of all the drug product chemical entities. As well as their stability
- An assessment of the components of the solution for injection for their stability and compatibility
- Any potential extractables and leachables from the rubber plunger, rubber cap seal and glass cartridge, which on contact with the solution for injection could be potentially extracted into the drug product, need to be identified and quantified
- Whether heat treatment at, for example, 80, 100, 120 or 130°C has any negative effects on the various components; these include the rubber seal and plunger. Change in hardness/elasticity could have a deleterious effect on the container closure integrity and plunger sliding during drug product administration and, as crucially, the solution for injection
- Stability study data of three batches of the product to set the batch release and shelf-life specifications.
The most suitable manufacturing process is only proposed and validated once the results of the above investigations are completed and collated.
What differences can the sterilisation process make?
There is a general description in the regulations with regard to the components, articaine hydrochloride and epinephrine injection as a sterile solution in water for injection. But no mention of excipients, anti-oxidants, rubber closures and the manufacturing process to use.
Consequently, this is the same for both the aseptic and terminal sterilised products.
If the product is manufactured aseptically there is no detectable change in the assay. With articaine (38-42 mg/mL (3.8-4.2%), however, if manufactured via terminal sterilisation there is a loss of 0.1-0.2% due to the hydrolysis of the articaine to form articaine acid.
With epinephrine, similar analysis shows no detectable change when produced aseptically. However, it is heat labile and reacts with the sulphite/bisulphite to form epinephrine sulphonic acid. Such that about 5-6% is lost during the sterilisation process.
As a consequence, the terminal sterilisation process requires at least an additional 15% to compensate for this degradation. While an anaesthetic produced aseptically requires a 5-10% addition.
The anti-oxidant sulphites/metabisulphites react with any residual oxygen in solution to form sulphuric acid. Over time this lowers the pH of the content. And it reacts with the epinephrine to form epinephrine sulphonic acid.
These reactions are more pronounced and faster when the drug product is heat treated. For example sterilisation at 121°C for 20 minutes causes about 4-6% loss of the epinephrine. And about 15-20% loss of the sulphite/metabisulphite.
Is one manufacturing method better than the other?
Where heat treatment has no detectable effect on the chemical entities in the solution for injection and/or the primary container rubber components, then a terminal sterilisation process should be used.
Alternatively, where heat sensitivity is detected then an aseptic manufacturing process is indicated.
This rationale is given support by the fact that FDA-approved articaine with epinephrine dental anaesthetics have a 24-month shelf life when produced with an aseptic process. And 18 months when produced with a terminal sterilisation process.
So, the next time we routinely ask for ‘just a local’ we are much more aware of the detailed planning and care applied to the seemingly mundane cartridge cradled safely in the syringe.
*Orabloc (articaine and epinephrine Pierrel) is approved by FDA and EMA agencies. It is produced aseptically at an Italian manufacturing site. Orabloc is exclusively distributed in the UK by Dental Sky Wholesaler Ltd.


