 The final Prosthodontips column of the year from Zo Ali and Josh Sharpling is all about smile design.
The final Prosthodontips column of the year from Zo Ali and Josh Sharpling is all about smile design.
As patients are becoming increasingly aware of their appearance and the contribution their dentition makes, I am receiving more and more requests for aesthetically driven treatment.
In this month’s column, I will address some of the objective criteria of smile design. The aim is to help you assess patients immediately as they present in clinic.
Why is smile design important?
The single most important reason is to establish a goal together with the patient and the dental laboratory.
Once this process starts, it allows for effective and clear communication between all three parties. This sets the tone and foundations for success at the end of treatment.
Beyond basic communication there are still numerous reasons to take the time to design the patient’s aesthetic form:
- Motivate the patient
- Involve the patient in their own journey and decision-making process
- Establish treatment objectives with the patient and laboratory
- Guide the diagnostic wax up
- Allow intraoral mock up
- Identify problems and complexities at an early stage in the patient’s journey
- To have an objective point of reference at each stage of treatment.


When assessing patients and considering aesthetic treatment, it is important to have a systematic approach to clinical assessment. This will ensure nothing is left out and will improve your efficiency as you repeat the same steps each time.
The approach I follow is:
- Extra oral (including facial analysis)
- Intraoral.
The concept is to essentially start large and slowly focus closer and closer on the mouth and teeth. This way we can build a better holistic picture of aetiology and potential for improvement.
Recording every stage of assessment using clinical photographs and videos is extremely important. It allows us to refer to these later and offers far more information than any traditional clinical note taking.
Extra oral assessment
I begin by generally looking at the face (Figure 3). The main features I am looking at are:
- Facial centrelines
- Facial height
- Skeletal relationship (anteroposterior)
- Symmetry
- Incisor show at rest
- Gingival display during smiling
- Occlusal plane
- Versus interpupillary line
- Versus Camper plane
- And versus Frankfurt plane.
Most of this can be done whilst simply getting to know the patient and during friendly conversation at the start of the appointment. It helps to have the patient relaxed by creating a nice atmosphere in the dental surgery. Make sure it is calm with no background noise. Perhaps some music and with no distractions in the patient’s field of vision.
This allows both the patient and clinician to engage fully in a meaningful way.
Absolutely symmetry is not a must. Indeed it does not exist (at least not that I have seen).
There is asymmetry in everyone’s face and dentitions. It is important to identify this early to aid aesthetic diagnosis and treatment planning.
Once identified, asymmetries can be photographed and discussed with the patient in an open manner.
Their impact on the care provided can be determined. And we can optimise our treatment approach before an impression is ever taken.
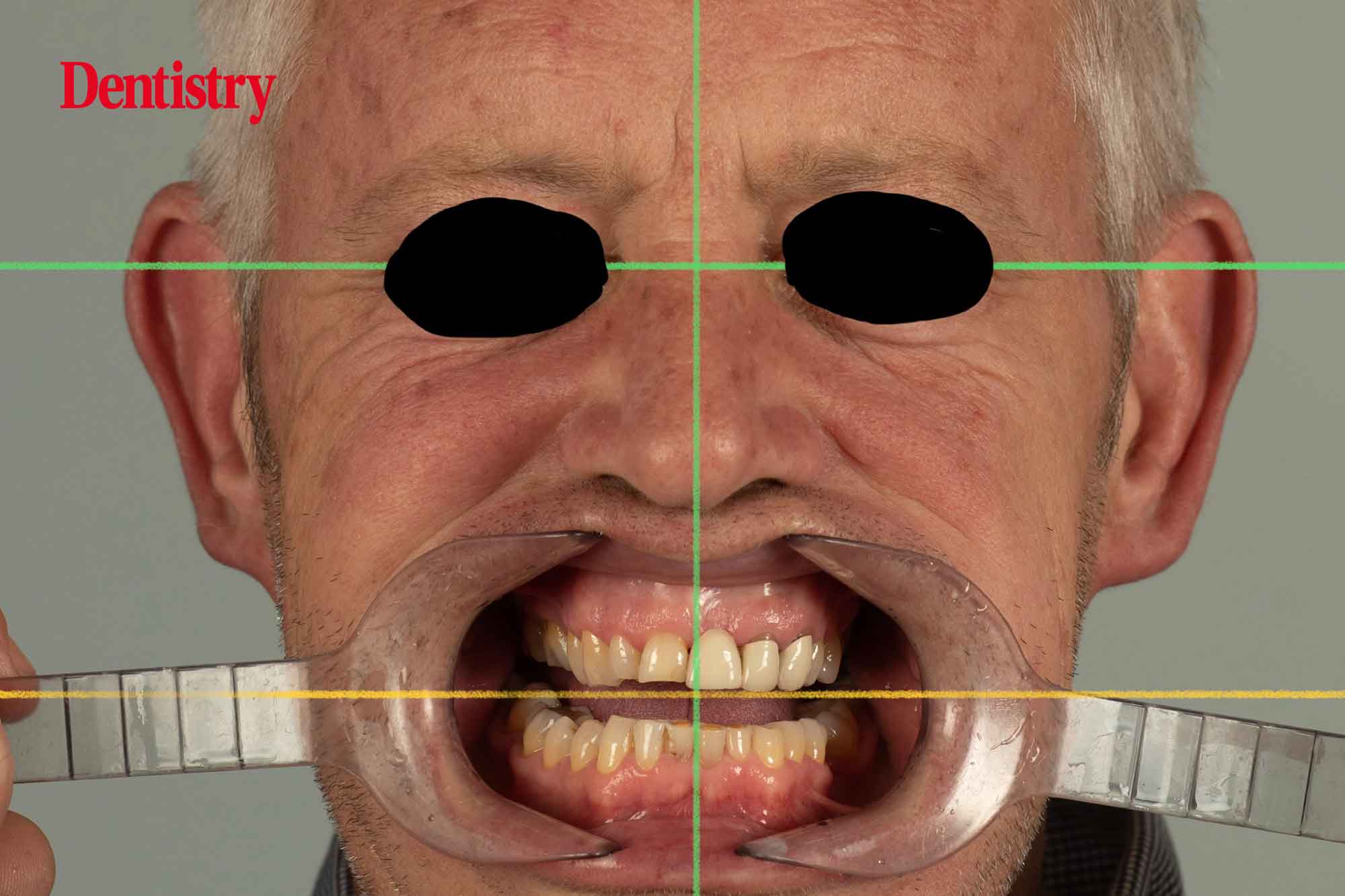
At the very least, assess the incisal display at rest and gingival display at smiling for every case. This gives us vital information of the relationship between the maxillary incisal edges and the lower lip.
The gingival display during smiling determines the importance (or lack thereof) of the soft tissues and periodontal condition to overall smile.
Intraoral assessment
Again, find a system that works for you and stick to it. I carry out my assessment in the following order:
- Soft tissue health
- Oral hygiene
- Basic periodontal examination
- Occlusion
- Comments on the restorative status of relevant teeth and the dentition in general.
Remember in most patients, at least 50% of the final aesthetic outcome is periodontal.
It is therefore an extremely undervalued part of smile design and aesthetic treatments.
Ideal gingival zenith position, exposed roots and pontic site development are all aspects of care that we ignore far too often.
A major part of the value of the periodontium is the presence of the interdental papilla. Only when we lose it do we really begin to realise the negative consequences of poor gingival health.
Objective criteria
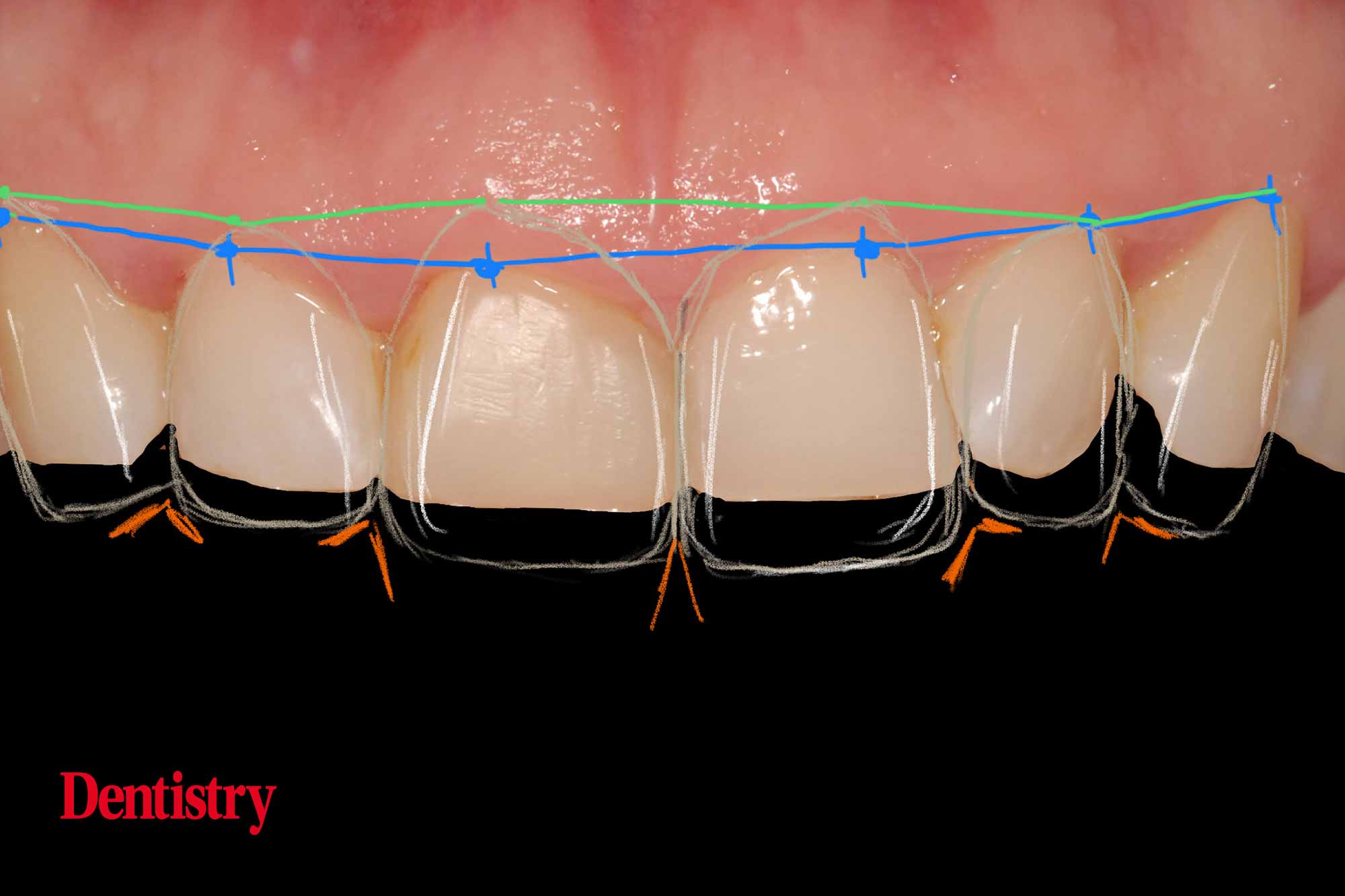
Finally, we look at some more objective criteria relating to the teeth themselves (Figure 4):
- Tooth axis
- Teeth should be slightly distally inclined
- Gingival zeniths
- The highest point on the gingival margin should be slightly distal to centre on the maxillary incisors but can lie more centrally on all other incisors and canine teeth
- They should be balanced so that the central incisor and canine are slightly more apical than the lateral incisors
- Basic tooth form
- We create this by having the basic correct outline of the tooth. And further refine it by the correct use of transitional line angles
- Surface texture
- This relates to the gloss and lustre of the teeth and/or restorations. It is important to match to adjacent teeth so as to produce similar light reflects
- Aged and worn teeth are generally far more polished than in dentitions of younger patients
- Colour
- Hue, value and chroma are the main determinant
- Value is of greatest importance and is related to surface texture (owing to light reflections)
- Incisal edge positions
- Currently, more patients are requesting straighter incisal edges as opposed to the more natural staggered position
- Straighter, more even edges contribute an aged or worn appearance however. Communicating this to patients is challenging
- Lower lip line
- The lower lip should be in very close proximity to the maxillary central incisor and canine edges during smiling.
Please keep the questions coming for the Prosthodontips team. You can contact us on Instagram (@sharplingdental and @prostho_zo) and also email ([email protected]).
If there are specific topics you would like us to cover in a column, please let us know.
Previous Prosthodontips:
- Restoration of a lower second molar
- Resin-retained bridges: fun and predictable
- What’s the solution to occlusion confusion?
- Dental ceramics
- Immediate dentures.
Follow Dentistry.co.uk on Instagram to keep up with all the latest dental news and trends


