 Join Zainab Al-Mukhtar as she takes over Dentistry’s Instagram account all day today and covers facial aesthetics and complications.
Join Zainab Al-Mukhtar as she takes over Dentistry’s Instagram account all day today and covers facial aesthetics and complications.
My reasons for incorporating ultrasound imaging to my clinical practice for hyaluronic acid injectable treatments in facial aesthetics has been to increase safety.
With rising facial rejuvenation procedures involving volume restoration, facial contouring and the revolutionary non surgical rhinoplasty with filler augmentation, safety is even more a priority. Emerging data and equipment makes management of complications more predictable.
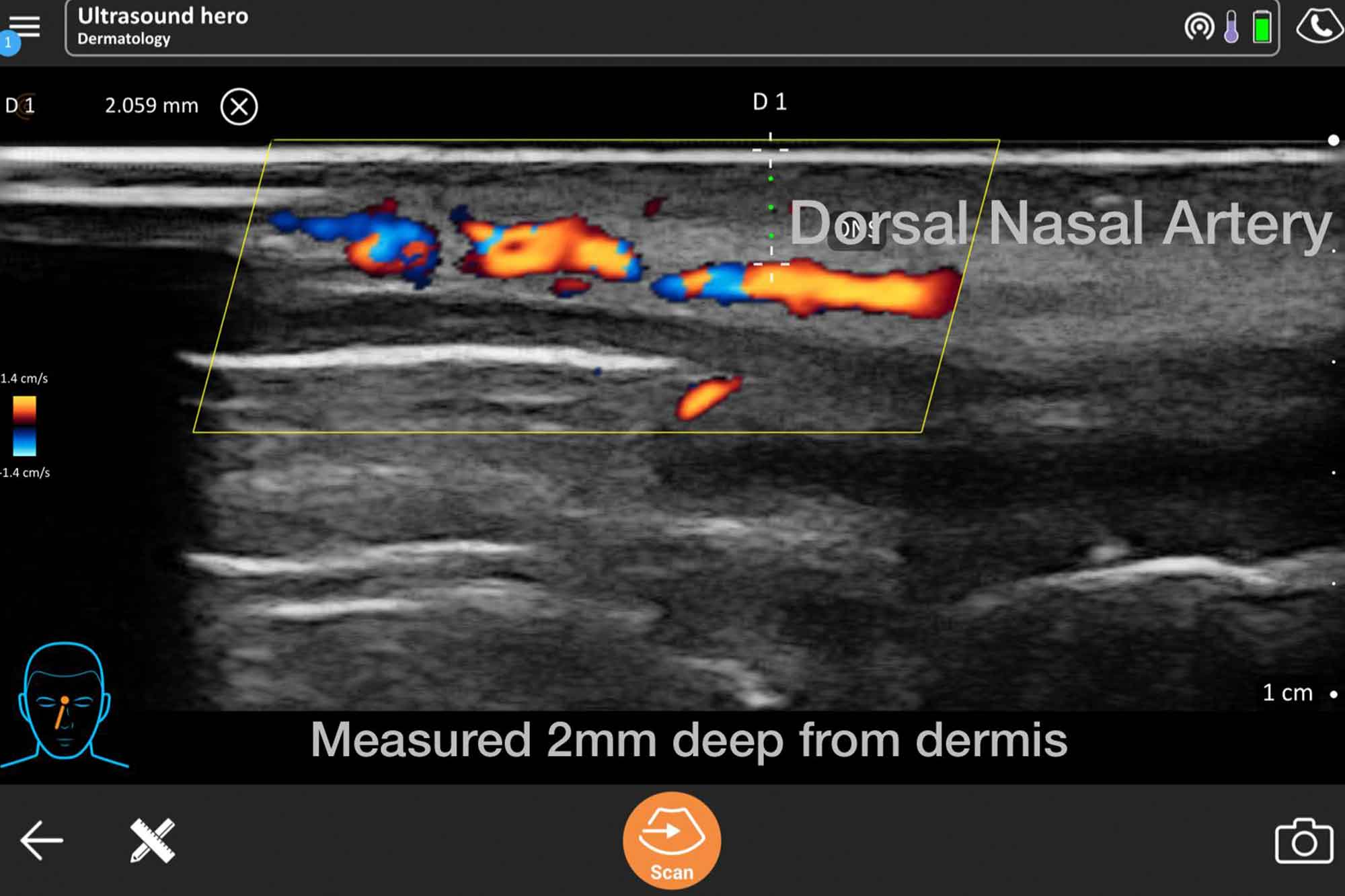
Ultrasound scanning (USS) is a non invasive way to visualise tissues under the skin. Adding doppler allows the detection of blood flow.
Interest in doppler ultrasound analysis of the face has grown, particularly for injectable fillers. Ultrasound is a valuable tool in the treatment of filler complications.
One of the rare but serious complications of filler treatments is a vascular occlusion (VO), in which the filler obstructs an artery. This causes restriction of oxygenated blood flow to tissues.
If left untreated, this leads to ischaemic necrosis (tissue death). The consequence can vary from mild scarring to significant disfigurement.
Emergency dissolving of filler is essential to unblock the obstruction, resuming normal blood flow to the deprived area.
Facial aesthetic complications
With doppler USS we can detect the precise location and depth of the problematic filler by assessing where there is a disruption in normal blood flow. We can then target this filler under ultrasound guidance and dissolve with hyaluronidase.
Without ultrasound, clinicians can flood tissues with high volumes of hyaluronidase, without precise location of the blockage. Reversal is still successful, but cases often need several repeated daily sessions injecting high volumes of hyaluronidase (traumatic for the patient and stressful for the clinician).
When unusually complicated vascular occlusions occur, this is challenging to resolve, despite high hyaluronidase volumes. This is due to the ambiguity of the exact location of the culprit filler bolus.
After supporting a few colleagues, who resorted to referring for ultrasound imaging during complications, I began training in ultrasound.
Under USS guidance, dissolving is with precision, lower hyaluronidase doses, less trauma, and the reassurance of continuous blood flow to the affected area.
Case study
Incidentally, a colleague referred a lovely patient to me with necrosis in her nasal septum after filler injection at a different clinic in London.
The clinician injected filler at the nasal spine to lift the nasal base. The injector did not recognise the early unusual symptoms that the patient experienced.
Necrosis in the septum is more rare with only one case report globally. This is unlike skin necrosis on the nose, which is more widely reported.
There were no obvious signs of skin abnormality. The patient’s unique symptoms were:
- A nose bleed immediately after filler injection
- Severe tooth pain on an upper left molar affecting sleep and needing painkillers for several nights
- Blood-stained dry crusting inside the nostril and a ‘stuffy nose’.
There was necrosis inside the left side of the nose in the nasal septum.
Dental and radiographic examination showed no tooth abnormality. This combination of signs and symptoms suggested a possible blockage in the septal branch of the superior labial artery and the Kiesselbach plexus.
Amazingly, after dissolving filler at the nasal spine with hyaluronidase under ultrasound guidance, the molar pain immediately disappeared.
Targeted dissolving continued until all symptoms were relieved. At the final scan, I involved global expert on facial ultrasound Dr Leonie Schelke in Amsterdam via video call. We looked carefully for any filler remnants.
One more guided dissolve and vascular occlusion was entirely reversed. A stark improvement in blood flow was seen on the doppler ultrasound image.
The patient was followed up with ENT doctors to confirm septal wound healing. This patient was very fortunate to have rapid ultrasound guided dissolving to reverse her complication.
The future of ultrasound imaging
We can also use facial USS for:
- Vascular mapping before or guided injections during filler placement, to prevent intravascular injection
- Optimising aesthetic results
- Monitoring filler changes over time.
Ultrasound imaging is most useful to experienced injectors. A very good understanding of facial anatomy is essential in order to interpret scans successfully. Clinicians also require training to understand ultrasound, and there is a learning curve.
Skilful scanning, confidence and interpretation comes with ultrasound experience. This therefore takes extensive commitment of time scanning patients routinely.
It is worthy of note that clinicians require finances, training and time investments to use facial USS successfully. For routine use, especially for beginners, clinicians also need additional appointment time.
Many predict that within a few years ultrasound imaging will become standard practice in cosmetic medicine, and time will tell.
To keep up with Zainab Al-Mukhtar during today’s Instagram takeover, simply follow @dentistry.co.uk.

