Proper communication can aid a practice looking to up its private production. Dr Derry Rogers and Dr John Renshaw explain how.
Whether UK dental clinicians are pressured by time and financial reward constraints to get their work completed, or whether there is less commitment within the GDC and its CPD requirements to continue the pursuit of clinical standards; we believe there is a definite crisis looming in the reputation of UK dental services.
Part one of this series of two articles will aim to explain the role that understanding communication systems plays in transitioning a dental practice from survival, through growth, to profit. This article will present ways to assist dental practices to move towards a more communicative, co-diagnostic based set of systems to create increased case acceptance with private treatment recommendations.
There are three differing subgroups in the pure private practice model.
‘Aside from the cost challenge associated with operating as a small business, the current small practice model is already under pressure, with many dentists approaching retirement age, a lack of newly qualified professionals to replace them, and a substantial number of younger (often female) dentists preferring to work part-time and therefore reluctant to own their own practices’ – KPMG, The Dental Chain Opportunity. 2017
Available statistics would suggest that the share of over £7.1 Billion (KPMG, 2017) gross dental revenue is spread over 43,000 plus registered dentists working in more than 12,000 practices, of which pure private practice makes up around 25%.
1: Mixed practice
The clinic delivers UDAs under an NHS-GDS or -PDS contract and also delivers clinical work outside the scope and financial constraints of UDAs via an independent, private practice model.
The patient is generally advised at the chairside prior to treatment, of the option to pay for higher standards of clinical care at an ‘out of pocket fee’ to the patient.
This type of practice often involves the principal delivering largely private-based care only and associates delivering the NHS treatment.
2: Private practice
Level 1: This Level 1 type practice may accept emergency patients, pain management, single tooth dentistry including extractions, fillings and root canals, depending on their business model (if in fact there is one). Scale and polish are more often delivered by the dentist, rather than a Hygienist or Therapist as often seen in Level 2 practices (a classic lack of delegation to well trained staff)
Level 2A: The clinic engages with the patient in a semi systematised way including verbal treatment plans for the single tooth issues they present with, and treatment recommendations are communicated to the patient in a generic process usually downloaded from the practice management software systems in use.
The practice is more organised than a Level 1 practice, often by the practice manager and the staff has a better knowledge of the standards of care the senior clinician wishes to deliver.
The team has more empathy in their patient care, better communication skills utilising photography (either intra-oral cameras or a digital SLR set up) and a desire to include newer CAD/CAM technologies to address the recommendations of the treatment plans presented.
Hygienists are more evident in these Level 2A practices and the staff have expanded roles to support the clinicians, thereby optimising the clinician’s time availability.
Bleaching is a common first step with hygiene treatment to initiate the patient’s awareness and involvement in their future dental health.
Level 2B: The practice engages more effectively with their patients through a highly systematised delivery process and photographic communication systems are the foundations that enable patients to see their own mouths with clear evidence of issues and recommendations. Photographic records are taken two-yearly with visual records updated after the completion of sequenced stages.
Full written treatment plans encompassing all diagnosed dental issues are provided with the sequencing of recommended care presented. This plan is then implemented and managed by the Treatment Coordinator.
Once the patient has completed part or all of their stages of treatment, they are placed in a “maintenance care and recall program’ under the guidance of the hygienist/therapist and overviewed by the clinician. At each recall the patient reviews with the clinical team their photographic records (which are updated at each stage of treatment completion) and any outstanding treatment is scheduled.
This practice can be totally systematised to deliver consistent care in an effective fashion by well-trained clinicians and teams delivering optimal profit levels.
The communication model
In 2012 the UK office of Fair Trading reported that dental patients often do not benefit from timely, clear and accurate information to make decisions regarding their choice of dentist or dental treatment.
‘82% of patients who recently received a course of dental treatment that incurred a charge did not receive a written Treatment Plan’ – Office of NHS
The more a dental practice engages with the move from an NHS-pays to a private-practice user-pays scheme, the more engaged with communication systems the clinical team needs to become as well as developing the ability to diagnose and present timely written treatment plans which should then become the norm for the transitioning practice. Successful communication leads to trust development and then case acceptance.
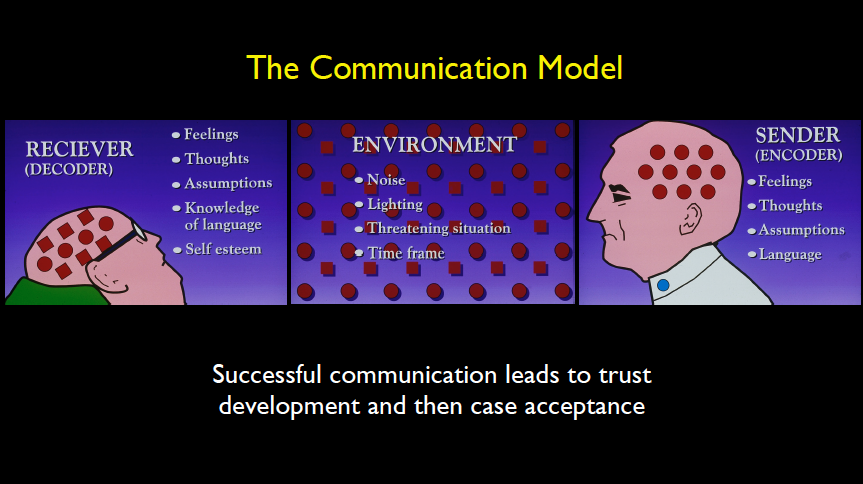
Figure 1 shows the traditional communication model in a practice showing the difficulties the environment creates in delivering clarity of explanation of simple and sometimes complex clinical situations.
The clinician is traditionally time poor and clearly influenced by their feelings and their thoughts at the time and their professional dental language is not clearly received by the generally nervous patient, who does not speak this strange tongue and, in the traditional challenging surgery environment does not grasp clearly what the clinician is trying to tell them.
Added to this communication nightmare are the differing personality styles of the clinician, the nursing team and the patients themselves.
The author has for many years taught ‘Personality profiling’ (as named by Dr Tony Aleksandra) and simplified it down to a basic set of four personality types defined by their emotive/openness levels (E) and their assertive/directness levels (A). (Figure 2)
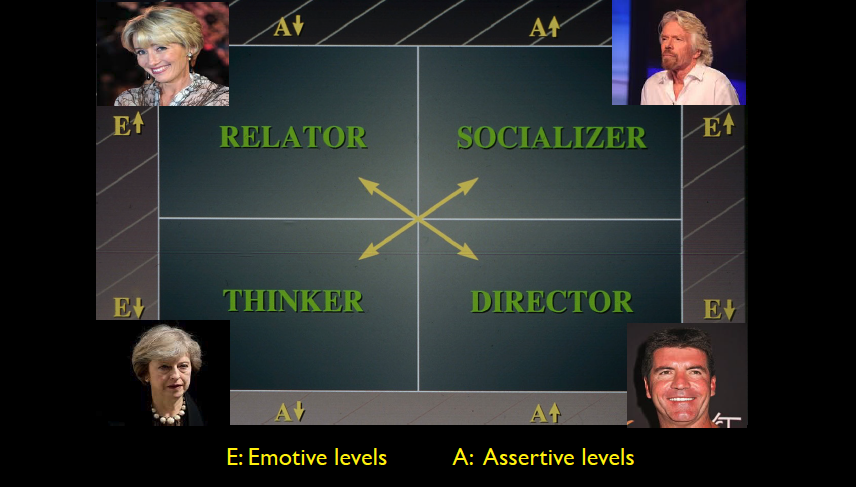
‘When people act and react in social situations, they exhibit clues that help to define their behavioural styles. You can identify behavioural style by watching for the observable aspects of people’s behaviour – those verbal, vocal and visual actions that people display when others are present.
Identifying personality styles is possible by classifying a patient’s behaviour in two dimensions: openness and directness. Openness (E) is the readiness and willingness with which a person outwardly shows emotions or feelings and develops interpersonal relationships.
Directness (A) refers to the amount of control and forcefulness that a person attempts to exercise over situations or other people, their thoughts and their emotions.’ – Dr Tony Allesandra, 1995
By understanding the personality profiles of the patient and the individuals in the clinical team, an opportunity to clearly communicate the way the patient is able to receive dental language is created. Trust development is initiated and a higher acceptance of treatment recommendations becomes the norm when utilised with the photographic records presentation.
The whole team needs to be trained in this very important skill, most importantly the reception team who are taking calls from new patients and existing clients either for recall exams or specific dental issues requiring care.
Evidence of shift to private practice
Private practice profits have crept ahead of NHS net profits for the first time in almost a decade. These figures come from the latest statistics released by NASDAL showing the average NHS practice makes a profit of £129,000 per principal compared with £131,000 for private practices.
Average gross fee income is up by £7,000 per NHS principal and £23,000 for private practice principals.
NASDAL has estimated that it costs £15,150 annually to meet CQC regulation requirements alone (this figure rises to £21,875 when registration fees and indemnity cover is added). The need to cover the costs of CQC compliance is increasing at an exponential rate (the cost of compliance for dental practices committing to CDC recommendations has risen by 1086% in the decade to 2016).
Clinicians need to look at increasing their net income through their private practice revenue to be able to afford these increasing costs, both to ensure patient safety and to maintain some semblance of lifestyle for themselves and their families.
With these trends showing a move towards private practice, it would serve both associates and principals to consider transitioning from a mixed practice model to an all-private model to provide greater practice income and hence improved quality of life.
The benefits of transitioning from mixed to private practice include:
• Better diagnosis from increased time availability to discuss treatment options
• Ability to engage with the patient using communication skills (Personality profiling) including photography techniques. This leads to better treatment planning and greater case acceptance
• Better quality of care delivery as a result of higher case acceptance levels combined with clinical training in newer technologies (such as the growing digital CAD/CAM systems).
We start to see the private practice clinician regaining control of their time via stress management and hence the ability to spend this time in patient communication, including treatment option discussions.
How to transition dental practices
The move from mixed to private practice is called the transition phase of practice growth.
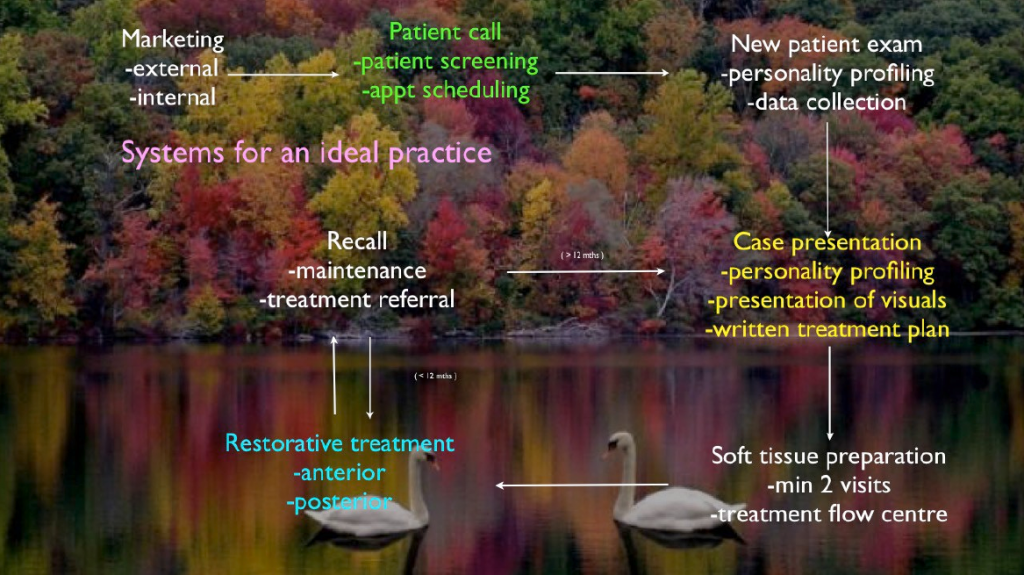
Such a transition requires a commitment on behalf of the well-led team to change the way they communicate with patients as well as a change in the way data is captured at the initial and recall examination visit via photographic visual records. Not all clinicians are generally gifted with the ability to communicate clearly and concisely in a world of time constraints and fee constraints (NHS practice), they would benefit from simple photographic procedures to capture the patients dental state in a way they can see for themselves what clinicians are trying to communicate.

Traditionally, students did not enter dental school on the basis of right brain skills. The entry process is based on the ability to pass ‘A’ level exams creating an assessment of intelligence rather than the emotional intelligence skills of the right brain that enable us to perceive and understand emotions.
Teams need to be trained and led with a clear vision (the ‘why’ of a the dental practice’s existence) presented to them clearly and the staff need to feel there is value in the change in direction of their practice from a reactive mode of treatment (presenting treatment for the problem tooth) to a more inclusive mode of communicating with the patient to develop their treatment plans.
By combining awareness of emotional intelligence, empathy, and knowledge of Personality Profiling, the clinical team can communicate effectively and accelerate trust development. Only after this has been achieved can case acceptance occur. It is paramount that the foundations of sound diagnosis and ethical treatment planning underpin it.
By understanding the Personality Profiles of the patient and the individuals in the clinical team, an opportunity to clearly communicate the way the patient is able to receive dental language is created.
Trust development is initiated and a higher acceptance of treatment recommendations becomes the norm when utilised with the photographic records presentation.
The whole team needs to be trained in this very important skill, most importantly the reception team who are taking calls from new patients and existing clients either for recall exams or specific dental issues requiring care. This is the point at which the day’s schedule is set up and stress levels are either created or defused.

The transition process needs systems to be developed by the team for the team and managed by the team. They then commit to this process so that the delivery of the patient care becomes systematised and consistent on at least an 80% eventuality basis.
This consistency of care combined with complete diagnosis and written treatment plans is what will lead to word-of-mouth referrals and a greater acceptance of recommended treatment; hence the transition to a more ideal practice where the clinicians and their team are remunerated for their time and skills in a caring empathetic environment that rewards the team with better quality of life.
It should be noted that transitional a practice places extra demands on a principal’s time; the time spent on vision and strategy to deliver that vision increases so the clinician is forced to delegate to other staff or take time out of their clinical time to manage the transitioning practice (Figure 4). It is a well know anecdotal point that the five-day-a-week clinician can be more effective and productive in four clinical days without extending their working hours.
The Ideal practice (Figure 5) receives its referrals from both internal and external marketing activities, it has a consistent and reliable system to collect photographic records, X-ray records and periodontal records. It provides written recommendations via the treatment plan after thorough diagnostic evaluation and this is presented to the patient in a clearly communicated process by a caring and empathetic dental team using Personality Profiling communication skills under the vision set out by the senior clinician/practice owner/practice manager as defined by the practice’s why!
Conclusions
• The stress of time demands and falling profits in dental practice due to increasing overheads are leading many dentists to consider early retirement due to stress and poor lifestyle.
• There will be a shortage of dentists to fulfil the roles required to create profitable corporate and independently owned practices
• By developing internal systems with their dental teams, practices can communicate more successfully via photographic records with their patients and hence increase the level of private practice ‘user pays’ revenue through a transitioning process.
Read part 2 in the February issue of Private Dentistry
 Dr Derry Rogers
Dr Derry Rogers
Dr Rogers qualified from the University of Melbourne in 1977 and is the founder and past president of the Australian Society of Dental Aesthetics. He is the managing director of CD Marketing and the clinical director of The DR Institute, lecturing and consulting extensively around the world.
Website: www.drinstitute.co.uk

Dr John Renshaw
Dr Renshaw is a former chairman of the BDA, has been a GDP for 47 years and is now retired from private practice in Scarborough. He consults with Oral Care Consulting, specialising in dental practice management, primary care dental service commissioning issues, legal compliance within the practice, complaints resolutions and wider healthcare policy. He has been a major player in dental politics for over 30 years and was chairman of the BDA from 2000 to 2006.
Website: www.oralcareconsulting.com


