 In this month’s Implant Insights column, Morven McCauley assesses the use of ISQ devices, including their accuracy, cost and benefits.
In this month’s Implant Insights column, Morven McCauley assesses the use of ISQ devices, including their accuracy, cost and benefits.
The use of resonance frequency analysis (RFA) devices to measure the implant stability quotient (ISQ) has significantly increased over the last five years in general practice.
But is it worth the expense and effort to provide a reliable indication of success of both primary and secondary stability?
What is ISQ?
The implant stability quotient (ISQ) is based on the objective RFA reading.
It is presented as an ISQ value of 1-100. The higher the ISQ, the more stable the implant.
The measurements can be repeated in a dynamic, non-invasive way to monitor the progress of osseointegration and secondary stability.
Along the implant-bone interface, it measures the stiffness of bone contact along the implant body.
How does it work?
Ostell state: ‘The technology is based on the tuning fork principle. A new peg is attached to the implant and made to vibrate, just like a tuning fork.
‘The purpose is to find the resonance frequency, ie the frequency with the strongest vibration.
‘The higher the resonance frequency, the higher the ISQ value and the more stable the implant is. This measurement is done quickly; it takes only a few seconds and is non-invasive.’
Why bother?
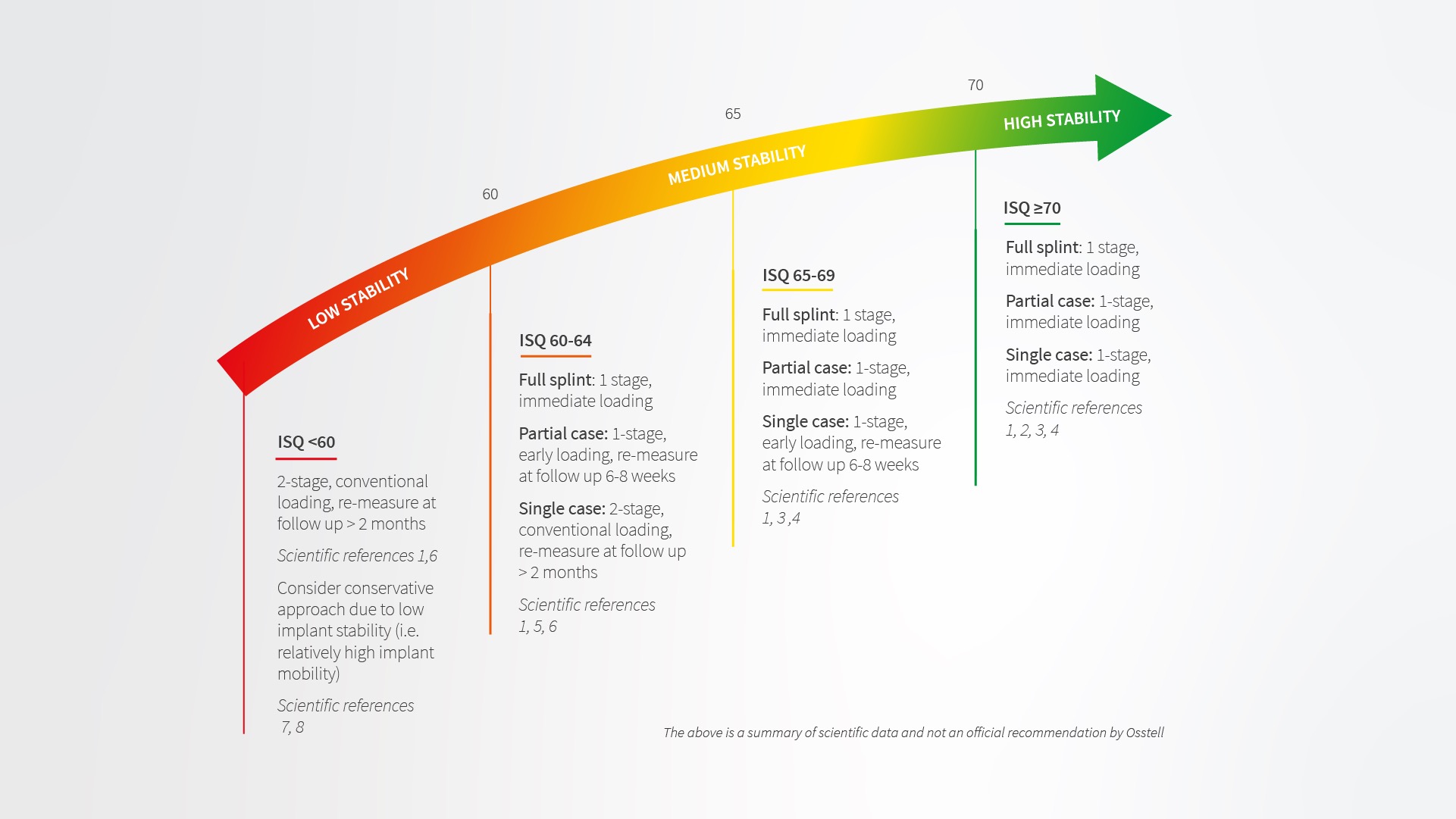
ISQ values are utilised to determine the implant stability and therefore, as a tool to calculate the optimum timeframe for implant loading as per the diagram illustrated below. This has the benefit of avoiding premature loading of an unstable implant.
Conversely, it also avoids unnecessarily long healing periods. The overall aim of this is to achieve more predictable and successful outcomes while being clinically efficient.
The value can also be utilised as an early indicator for ultimate implant failure.
Additionally, ISQ devices help enhance the communication we have with our patients and develop trust in the relationship. With the presentation of the ISQ readings of their implant, they may have greater understanding. Therefore, they may be more accepting of the decision for delayed loading and/or an extended healing period.
The declaration of ISQ readings also holds great benefit for case documentation, quality assurance and auditing purposes.
But how accurate is it?
More than 1000 articles on the subject have been published in peer-reviewed papers since 1996. The majority of these articles look into the array of clinical and biological factors that can influence the ISQ values.
Huang, Wu and Hunziker’s 2020 literature review provides a fantastic analysis and overview of these factors. Their study found 13 ISQ-influencing factors with the most evidence relating to implant location, bone density and gender.
In addition, the mandible, Type D4 bone and the male sex all retrospectively provided higher ISQ readings.
A common finding in these studies is that implants with low and/or decreasing ISQ values seem to pose an increased risk for failure. This is compared with implants with initially high and/or increasing values.
The cost of ISQ
There are currently two main RFA devices on the market in the UK:
- Penguin RFA – retails from £1,500 excl vat, with their re-useable Multipeg components from £26 each
- The Ostell range of devices, with their cordless Beacon device from £2300 excl vat and their single-use Smartpeg components from £17 each.
The re-useable Multipeg components are compatible with all devices, with careful reference to a conversion chart for equivalent ISQ values.
In summary, early in my implant career I have personally found the use of the Ostell Beacon a valuable device for assessment.
Firstly, this is because of its stability and ability as a tool in decision making on the selection of its loading protocol. Secondly, because of its indication to the predictability of the overall outcome of the implant.
A little pat on the back, reassurance and accountability for the clinical decisions that I have made. This is especially important in an era where a little more reliable evidence, validation and data can do no harm.
Catch Morven’s previous Implant Insights columns:
- Is implant dentistry the answer to the balance between work-life and mum-life?
- Inside the factory – implant edition.
Follow Dentistry.co.uk on Instagram to keep up with all the latest dental news and trends.


