 In the second part of the series, Kreena Patel and Amit Patel look at different methods to save compromised teeth. This month it’s single-visit crown lengthening and endodontics.
In the second part of the series, Kreena Patel and Amit Patel look at different methods to save compromised teeth. This month it’s single-visit crown lengthening and endodontics.
What is crown lengthening?
Surgical crown lengthening is a procedure that aims to expose sound tooth tissue by apical repositioning of gingival tissues, with or without removal of alveolar bone.
What are the indications for crown lengthening?
Crown lengthening surgery can be categorised as aesthetic or functional.
Ideally, the gingival display of maxillary anterior teeth should not exceed 2-3mm above the cervical area of a tooth (Kokrich, 1996). Approximately, 10% of patients have excessive gingival display when smiling (Tjan et al, 1984). This is more common in women and particularly noticeable if the patient has a high lip line.
Aesthetic crown lengthening can be used to remove this excess gingivae and help improve the appearance of short clinical crowns or uneven gingival contour.
Functional crown lengthening aims to gain adequate clinical crown height to restore teeth with subgingival caries, fractures or tooth wear. It allows:
- Access to the defect
- Ability to achieve moisture control for adhesive restorations
- Crown preparation lines can be placed on sound tooth tissue
- Impression taking
- Sufficient ferrule (ideally 2mm circumferentially) for more predictable long-term restorations.
What is biological width?
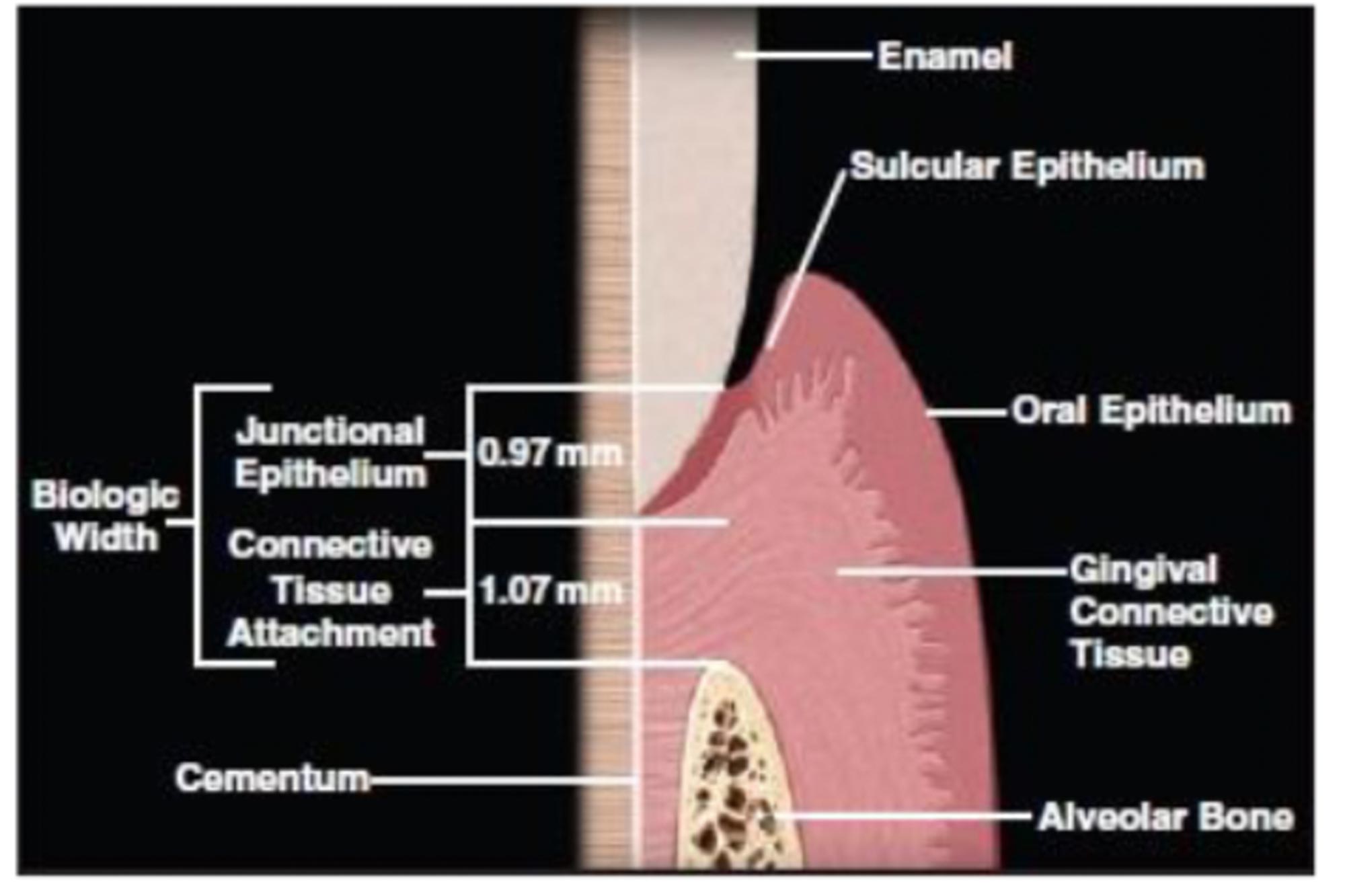
The biological width is defined as the dimension of the soft tissue, which is attached to the portion of the tooth coronal to the crest of the alveolar bone. This was defined by Gargiulo et al, who described the dimensions and relationship of the dentogingival junction. The new periodontal classification has now replaced the term biological width with ‘supracrestal tissue attachment’.
Gargiulio et al showed that the biologic width on average is 2.04 mm, which is the sum of the epithelial tissue attachment and connective tissue attachment measurements (Figure 1). If you take into account the gingival crevice then we have an average of 3mm for the biological width. This translates to limiting subgingival margin extension to approximately 0.5-1mm.
Essentially the biological width is important for the preservation of periodontal health.
Invasion of biological width can potentially cause chronic inflammation in gingivae with a thick biotype or recession in those with a thin biotype. Respecting the biological width for both aesthetic and functional crown lengthening will give you better long term results.
What are the risks of crown lengthening?
Crown lengthening of a single tooth may yield unfavourable aesthetic results, such as black triangles. Patients may also develop sensitivity to adjacent vital teeth.
As with all surgical procedures, the risks include postoperative:
- Pain
- Bleeding
- Swelling
- Infection
- Bruising
- Damage to adjacent teeth.
Emphasise the importance of good oral hygiene following the procedure.
Crown lengthening particularly in the aesthetic zone is challenging. It is important to consider referring the patient to a periodontist for management of cases the clinician feels is outside their competency.
What is the crown lengthening procedure?
There are many surgical techniques we can utilise for crown lengthening, such as gingivectomy in gingival hypertrophy cases or apically repositioned flaps in functional crown lengthening cases. A combination of these procedures may be required to perform aesthetic crown lengthening.
This article is focused on saving compromised teeth where crown lengthening is carried out to expose enough of the root so the restoration does not impinge on the biological width.
When crown lengthening on the buccal aspect, a three-sided flap is generally recommended to allow the flap to be apically repositioned. The main advantage of this technique is that you are moving the whole gingival complex apically without removing any of the keratinised tissue.
When crown lengthening on the palatal aspect, it is important to note that the palatal tissue cannot be apically repositioned as the tissues are fully bound down. In this situation the traditional periodontal technique of an inverse bevel incision works well (Figure 1).
The advantage of this technique is that you are performing a gingivectomy and thinning the palatal flap simultaneously. This allows the flap to naturally fall more apical to the margin of the new restoration.
Firstly, assess the amount of bone present around the tooth. We have to ask two questions:
- If we remove bone around this tooth will it compromise the long-term prognosis? For example, if it is a molar tooth, will we open the furcation by removing bone?
- Does the tooth have an adequate crown to root ratio for the final restoration to be successful?
Bone removal is usually performed using slow speed burs to help recreate the normal architecture of the bone, thereby re-establishing the biological width. High speed burs can also be used but the hand piece needs to be either an electric motor or rear venting to avoid the risk of surgical emphysema.
We prefer using the Acteon Piezotome unit, which has specific crown lengthening tips designed for this procedure (Figure 2).

Figure 2: Acteon piezotome cube, with crown extension tips
The gingival tissue are sutured using 5/0 or smaller sutures. These are removed two weeks after, following which a temporary crown needs fitting to help stabilise the position of the new gingival margin. It is ideal to do this during the surgery as the margins can be made smooth before closure of the tissue.
My top crown lengthening tips by Dr Amit Patel
- Assess the amount of keratinised tissue present. If there is less than 3mm then I would apically reposition the flap rather than preform a gingivectomy
- Use slow speed burs to remove bone
- Always root plane the tooth to remove all cementum and stop regrowth of bone
- Prepare the tooth for a restoration preferably at the time of surgery, or two weeks postoperatively
- Make a well fitting temporary crown to help control the gingival tissue at the new established level.
Single-visit crown lengthening and endodontics by Dr Kreena Patel
The crown lengthening procedure can be carried out at the same visit as the endodontic treatment and core.
The cases presented will discuss how the procedure is carried out:
Case one
Preoperative assessment
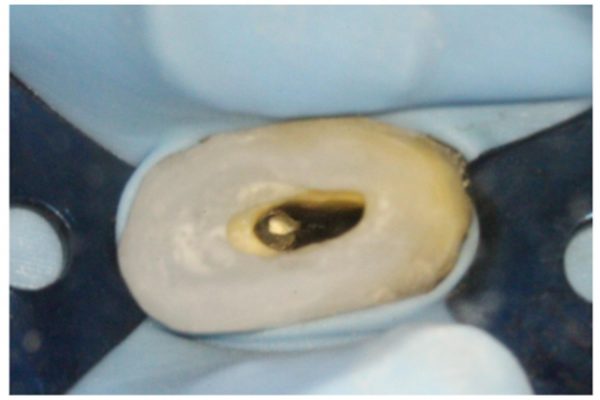
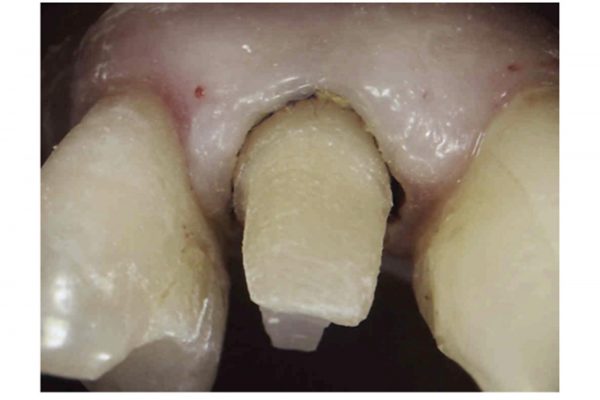
The patient presented with a fractured palatal cusp on UR5. Clinically, UR5 was restored with a MOD composite restoration, with a thin buccal cusp remaining (Figure 3).
In general, the patient had an extensively restored dentition, no evidence of periodontal disease and good oral hygiene.

Figure 3: Palatal cusp fracture
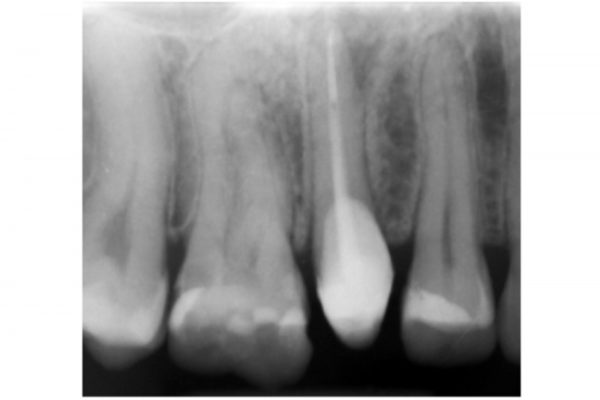
A periapical radiograph revealed there was limited tooth tissue remaining and a periapical radiolucency associated with UR5. The bone levels were normal and there was a favourable crown:root ratio (Figure 4).
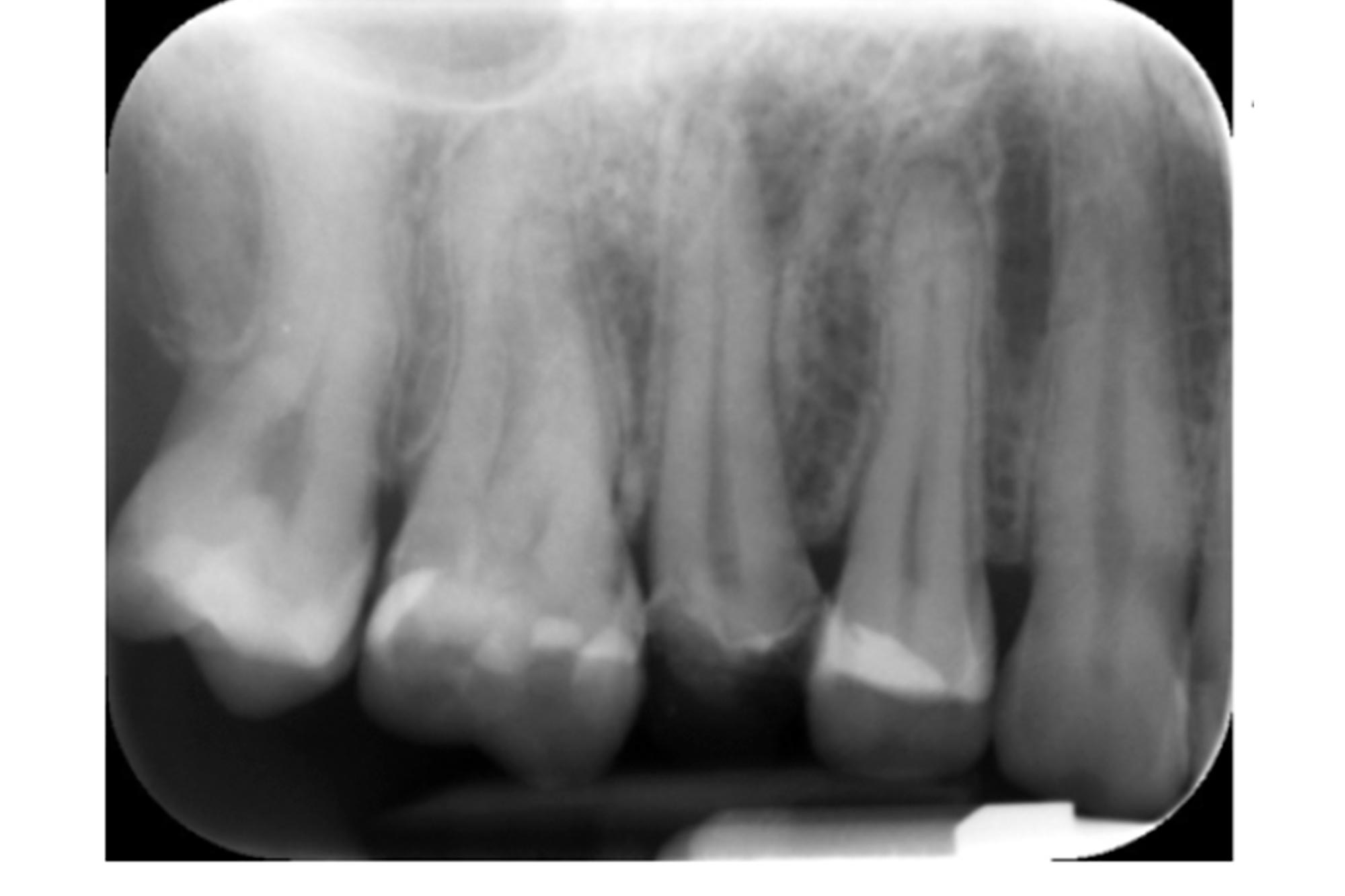
Figure 4: Periapical radiograph of UR5
Following the administration of local anaesthetic, the mobile fragment was removed using extraction forceps. The fracture extended into the coronal third of the root (Figure 5).
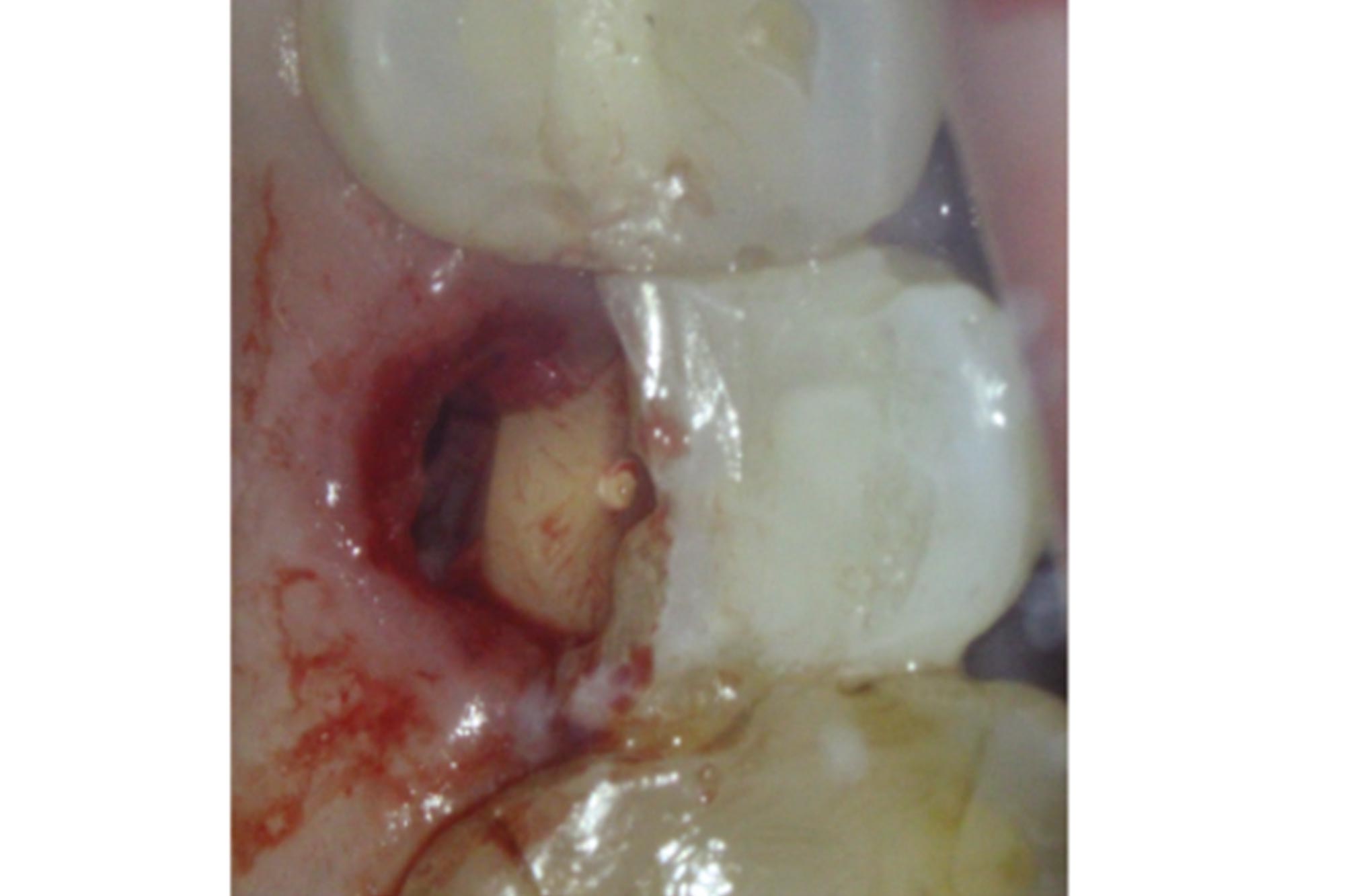
Figure 5
The following treatment options were discussed with the patient.
- Extraction – replacement options to include a denture, adhesive bridge or implant
- a) Restorability assessment b) Crown lengthening c) RCT and fibre post d) Cuspal coverage restoration.
It was emphasised that teeth with limited tooth tissue remaining have a more guarded long term prognosis. Option two would aim to save the tooth for as long as possible and delay the need for extraction.
The patient was keen to try to proceed with option two.
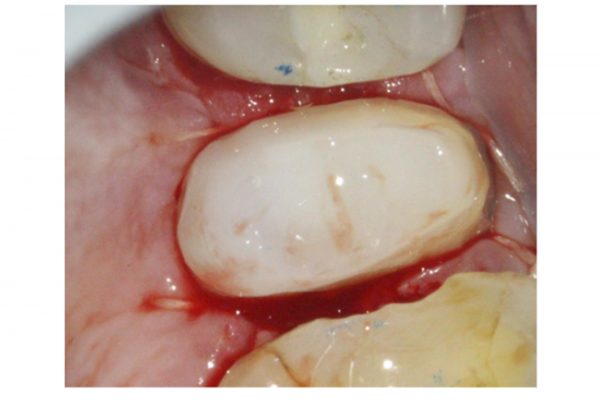
Crown lengthening procedure (Figure 6)
- The existing restoration and caries was removed. The tooth was found to be restorable if crown lengthening was carried out
- A gingivectomy was preformed using an inverse beveled incision (45 degrees to the long axis of UR5)
- A full thickness muco-periosteal envelope flap was raised from UR4 (mesial) to UR6 (distal)
- The flap was retracted using a Prichard periosteal elevator
- Bone was removed using a piezotome (Acteon Cube) using tips CE3 palatally and SL1 interdentally.
- Haemostasis achieved using sterile gauze soaked in adrenaline (100 micrograms/ml) packed under the palatal flap. This was replaced with dry gauze during the restoration placement
- A matrix band and wedges were placed around UR5. Good isolation and moisture control was achieved. A pre-endodontic composite restoration was placed
- Saline was used to flush the site and the flap sutured into position.
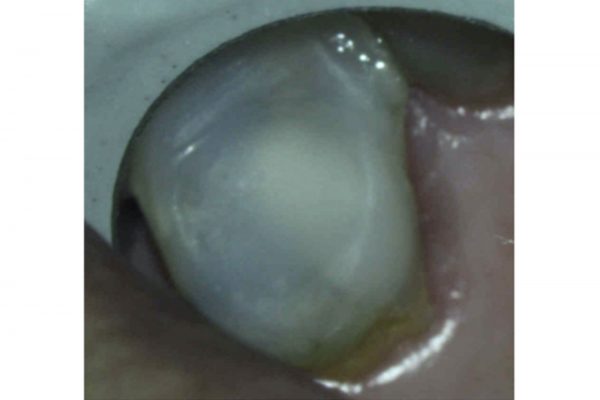
Endodontic procedure (Figures 6-7)
- A rubber dam was placed. Care was taken to ensure the clamp edges did not sit on the gingivae
- Root canal treatment was carried out; two canals were located and prepared using rotary files. The canals were obturated using warm vertical condensation
- A fibre post was placed in the palatal canal and cemented with a dual cure cement
- Composite core was placed
- Haemeostasis was confirmed and the patient was given postoperative instructions.
Review
The patient reported minimal postoperative discomfort. The patient maintained a very good level of oral hygiene and the gingivae was healing well. The stitches were removed (Figure 8).
A cuspal coverage restoration was recommended.

Case two
The patient presented with a fractured mesio-palatal cusp on UL6. Clinically, UL6 was restored with a MODB composite restoration. A periapical radiograph revealed there was a periapical radiolucency associated with the MB root. The bone levels were normal and there was a favourable crown:root ratio (Figure 9).
- A similar method was used as the previous case. However, in this case the full thickness muco-periosteal envelope flap was raised from UR6 (distal) to UR5 (mesial) and slow speed burs were used to remove bone (Figure 10).
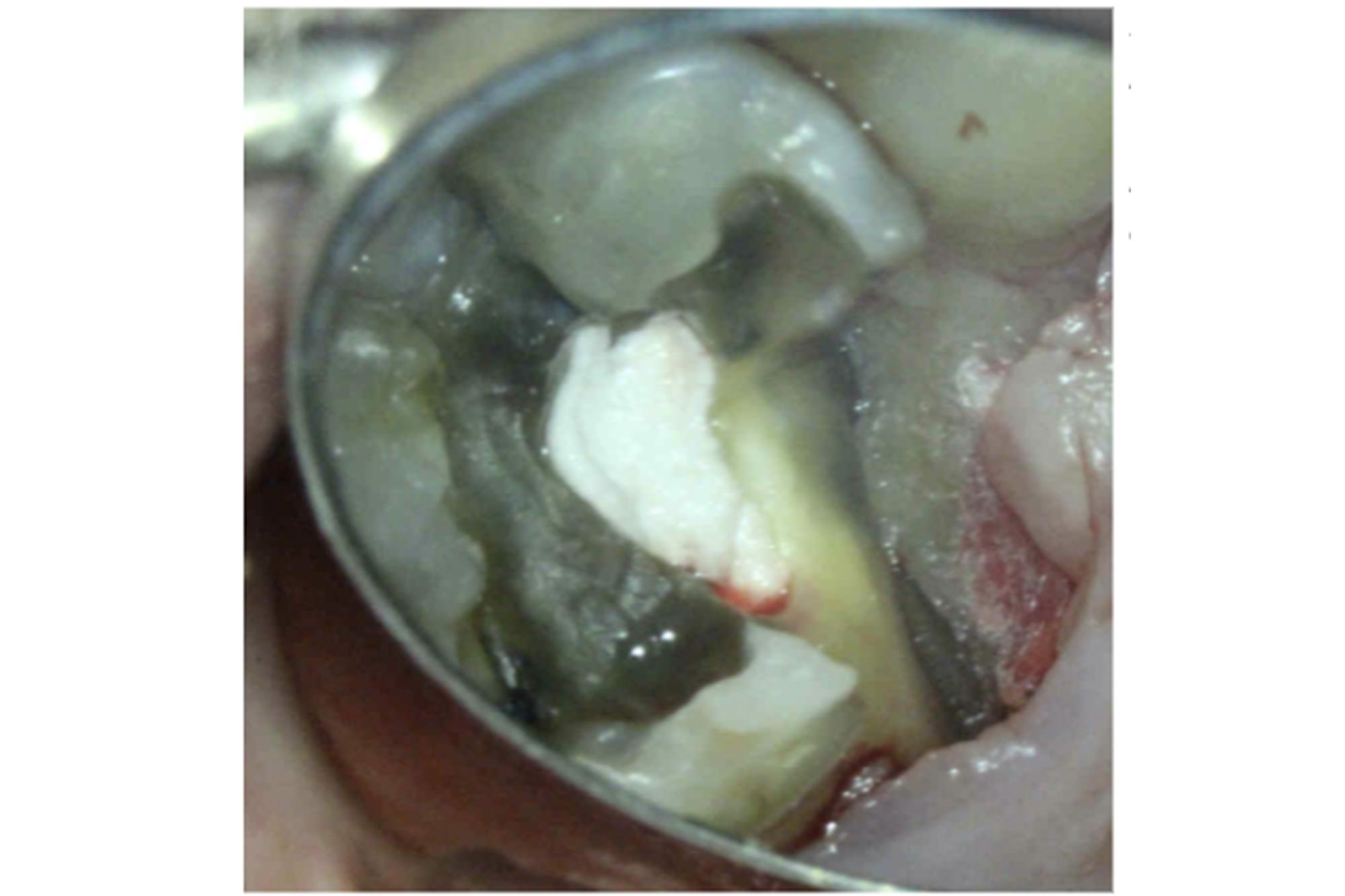
Figure 10: Full thickness mucoperiosteal flap raised from UR6 (distal) to UR5 (mesial). Bone removed using slow speed burs around the fracture site
- Following homeostasis, Opaldam was used to maintain haemostasis during restoration placement (Figure 11). This was removed prior to flap closure.
- Following the endodontic treatment, the composite core was extended 2-3mm into the canal orifices (Figure 12)
- A cuspal coverage restoration was recommended.
What are the benefits of single visit crown lengthening and endodontics?
A well-adapted restoration can be placed immediately which helps gingival healing.
Fewer dental visits and time are required to save the tooth making it a more viable treatment option with lower patient morbidity. It also saves the clinician time and the cost of the procedure may be reduced as a result.
What are the negatives of single visit crown lengthening and endodontics?
A longer treatment time is required to carry out crown lengthening and the endodontic procedure at the same visit.
Treated teeth may have less supra-gingival tooth tissue remaining, and may require a post supported restoration. Extensively restored teeth have a higher risk of fracture long term.
A small amount of bone removal is required for the crown lengthening procedure. This should not affect future implant placement as only a small amount of coronal bone is removed.
Postoperative care?
The patient should be advised not to rinse, drink alcohol or exercise on the day of the surgery. Hot foods should be avoided for 24 hours, and soft foods should be eaten for one week. Smoking should be avoided for seven to 10 days.
Ice packs are recommended (20 minutes on, 20 minutes off) for the first 48 hours to reduce swelling. Painkillers should be stated before the anaesthetic wears off. Alternating paracetamol and ibuprofen works well for pain relief and reducing inflammation.
The patient should maintain good oral hygiene but not brush the surgical site for one week. Salt water mouthwashes or chlorhexdinde mouthwashes are recommended three to four times daily for one week only, but only to bath the site and not to rinse as there is a chance the sutures may come undone. Interdental brushes can be started two weeks postoperatively.
The stitches can be removed one-two weeks following the procedure. Following this the tooth can be prepared for the definitive restoration, and a well-fitting temporary placed. This allows the tissues to mature around the new margin.
When should we place the definitive cuspal coverage restoration?
It is recommended to wait at least six weeks for full healing and gingival maturation prior to placing a definitive cuspal coverage restoration. If aesthetic crown lengthening is carried out it is recommended to wait three to six months.
How should I design the definitive cuspal coverage restoration?
Teeth requiring functional crown lengthening often have limited tooth tissue remaining. Therefore, it is important to preserve as much of the remaining structure as possible when designing the cuspal coverage restoration.
An onlay restoration may work very well in these situations. However, it can be more challenging to make these aesthetic buccally where the join between the tooth and onlay may be visible (Figure 13).


Alternatively, a monolithic zirconia crown with a verti-prep can be used (Figure 14).
The margins of the cuspal coverage restoration can be placed on sound tooth tissue. However, this can be challenging and potentially more destructive, particularly in situations where a greater degree of crown lengthening had been required. In these situations deep margin elevation may be preferred.
What are the alternatives to crown lengthening?
Deep margin elevation (DME)
This is where a direct restoration is used to raise the cavity margin to an equigingival or supragingival location. It has been used successfully as an alternative to functional crown lengthening in some instances. Please refer to ‘Saving compromised teeth part one: deep margin elevation’ for further information.
Current evidence shows DME appears to be well tolerated by the periodontium when carried out to a good standard. It has been shown to lead to very few to no signs of clinical inflammation (Safati and Tirlet, 2018).
Orthodontic extrusion
The time for extrusion varies depending on the amount of tooth extruded, and usually takes one to three weeks. An eight to 12-week period of retention is then required to stabilise the root in its new position (Simon et al 1978).
The procedure may result in the gingival margin and bone migrating coronally with the tooth during extrusion. This occurs due to tension produced by supracrestal fibres, and can result in the need for postoperative crown lengthening (Ingber, 1974). A gingival fiberotomy immediately before extrusion and weekly during activation may help prevent this, as well as reduce the need to longer retention periods (Weissman, 1983, Pontoriero et al, 1987).
Orthodontic extrusion is relatively complex and relies on close liaison between an orthodontist and restorative dentists. Treatment is costly and time consuming. It also requires patient compliance and can result in unfavourable aesthetics for the duration of the treatment (Dietrich et al, 2019). However, it is less invasive and there is no inference with the periodontium of neighbouring teeth.
Surgical extrusion, also referred to as intra-alveolar transplantation, is a procedure in which a tooth is surgically repositioned in a more coronal position within its own socket. It was introduced as a more rapid alternative to orthodontic extrusion.
The tooth can be carefully extracted using luxators, periotomes and forceps. Minimally invasive surgical extrusion can also be undertaken using the Benex extraction system. This provides controlled tooth extrusion with minimal deformation to the bone socket (Dietrich et al, 2019).
Conclusion
In the last few decades, the trend appears to be to extract compromised teeth and replace them with dental implants. However, with increased knowledge and long-term research, we know that dental implants are subject to biological and technical complications. Saving natural teeth can delay or prevent the placement of dental implants so the patient retains a fixed replacement for longer.
Functional crown lengthening allows us to save compromised teeth, and is an important treatment option which should be discussed and offered to patients.
References
Dietrich T, Krug R, Krastl G and Tomson PL (2019) Restoring the unrestorable! Developing coronal tooth tissue with a minimally invasive surgical extrusion technique. Br Dent J 226(10): 789-93
Gargiulo AW, Wentz FM and Orban B (1961) Dimensions and relations of the dentogingival junction in humans. J Periodontol 32: 261-7
Ingber JS (1974) Forced eruption: Part I. A method of treating isolated one- and two- wall infrabony osseous defects—Rationale and case report. J Periodontol 45: 199-206
Pontoriero R, Celenza F Jr, Ricci G and Carnevale G (1987) Rapid extrusion with fiber resection: a combined orthodontic-periodontic treatment modality. Int J Periodontics Restorative Dent 7(5): 30-43
Simon JH, Kelly WH, Gordon DG and Ericksen GW (1978) Extrusion of endodontically treated teeth. J Am Dent Assoc 97(1): 17-23
Amit is the principal specialist and director at Birmingham Dental Specialists in Birmingham. His special interests are dental implants, regenerative and aesthetic periodontics.
Amit graduated from the University of Liverpool and completed a four-year specialist training programme in periodontics at Guy’s, King’s & St Thomas’ Dental Institute. Amit was an associate specialist in periodontics at the Birmingham Dental School for nine years and is still an honorary clinical lecturer at the University of Birmingham School of Dentistry. He has taught at undergraduate and postgraduate level, including lecturing to dental practitioners both in the UK and internationally. Amit is also on the committee of the Association of Dental Implantology and the president elect.
Follow Dentistry Online on Instagram to keep up with all the latest dental news and trends.
If you would like to learn more about endodontics follow Kreena on Facebook and Instagram @kreenaspecialistendodontics.