Follow Dentistry.co.uk on Instagram to keep up with all the latest dental news and trends.
 The coronavirus (COVID-19) pandemic represents a challenge to all healthcare. Due to the nature of dentistry, social distancing is impossible when treating patients face to face for emergency dental procedures. Many in the dental community feel helpless, unable to satisfactorily help patients in need, and feel that the guidance from our governing bodies has been inadequate. In this article Kris Leeson and Robert Lewis will discuss the journey that Thorpe Dental Group has taken to help patients in need, whilst still following current best practice in an ever changing world of dentistry.
The coronavirus (COVID-19) pandemic represents a challenge to all healthcare. Due to the nature of dentistry, social distancing is impossible when treating patients face to face for emergency dental procedures. Many in the dental community feel helpless, unable to satisfactorily help patients in need, and feel that the guidance from our governing bodies has been inadequate. In this article Kris Leeson and Robert Lewis will discuss the journey that Thorpe Dental Group has taken to help patients in need, whilst still following current best practice in an ever changing world of dentistry.
Aims
- Discuss the journey in setting up a private emergency dental hub
- Discuss remote triage and advice, analgesia and antibiotics (AAA)
- Discuss the required personal protective equipment (PPE) for aerosol generating procedures (AGPs)
- Highlighting the difficulty brought on by this new way of working.
Objectives
- Developing a standard operating procedures (SOP) document, which is tailored to an individual dental practice
- Consideration of regulatory bodies
- Creating a cluster of dental practices.
Introduction
As healthcare professionals our primary concern is the wellbeing of our patients. During these unprecedented times, caring for our patients has been almost impossible.
Why is this?
From the end of March 2020 most dental practices closed due to the risk of transmission of COVID-19. The main concern was from AGPs and the risk to both the dental team and patients.
During her webinar on the 3 April, the CDO said no dental practices should be continuing to carry out any face to face treatment after the NHS urgent hubs had opened. Unfortunately, these hubs did not open all at the same time. Many dentists found them difficult to access. Referrals have to be sent via an NHS email account, which some private practices have struggled to obtain, despite the fast-tracking of applications. Some also found that no emergency hubs were available in their area. Further to this, anxious patients may not feel comfortable seeing a different dentist, and clinicians may feel that they are best placed to treat their own patients, having access to their dental histories and radiographs.
Remote triage and AAA
From lockdown, dentists were advised to stop face to face consultations and help our patients over the phone only, following AAA. This included antibiotics if appropriate. If this approach did not help the patient, then a referral to an urgent dental hub was indicated. A lack of PPE has meant that many of these hubs are only able to complete non-AGP procedures, so a patient in pain would only be able to have an extraction.
- Life-threatening emergencies, eg airway restriction or breathing/swallowing difficulties due to facial swelling
- Trauma including facial/oral laceration and/or dentoalveolar injuries, for example avulsion of a permanent tooth
- Oro-facial swelling that is significant and worsening
- Post-extraction bleeding that the patient cannot control with local measures
- Dental conditions that have resulted in acute and severe systemic illness
- Severe dental and facial pain: that is, pain that cannot be controlled by the patient following self-help advice
- Fractured teeth or tooth with pulpal exposure
- Dental and soft tissue infections without a systemic effect
- Suspected oral cancer
- Oro-dental conditions that are likely to exacerbate systemic medical conditions.
Our journey to opening a private UDC
We opened our private UDC on the 11 May 2020. We felt that patients deserved to be seen quickly and not be left with a period of worry and/or pain. And so we decided that setting up a hub was in the best interests of the patients within York, where there are many private practices.
It should be stressed that clustering a number of practices together to provide this service was one of our main criteria to help to reduce person to person contact as much as physically possible. There are 14 practices within the hub, responsible for approximately 22,000 patients.
Initially, we had been locked down for a three-week period, and we could accept that most dental conditions could be left for this time and managed appropriately with remote triage and AAA. As the lockdown continued with no definitive end in sight, we believed many patients’ dental issues should not be left. They may seriously impact upon mental and physical wellbeing. Some patients have been left unable to be seen by the NHS hubs without first being given multiple courses of antibiotics. Even when symptoms do not suggest an infection.
Video calling using Whatsapp was a useful way to remotely assess patients. This was not always possible, but was a great help in determining patients’ facial expressions and demeanour. It helped to judge the level of pain patients were experiencing or the severity of any facial swelling.
As the lockdown continues, the list of emergency dental procedures needs to be re-evaluated. Dental implant emergencies were never discussed in any NHS guidance, but issues like lost abutments, lost crowns and fractured temporary prostheses can have a detrimental effect on the longevity of dental implants. Following remote triage, we used our clinical judgement when deciding which conditions warranted face to face treatment, putting patients’ interests first and only offering appointments when it was safe to do so.
It was decided that we would see patients in the following categories, if deemed appropriate:
- Category two – patients who are shielded – those who are at most significant risk from COVID-19
- Category three – patients who are vulnerable/at increased risk from COVID-19
- Category four – patients who do not fit one of the above categories
- Category one – patients would need to be seen at a COVID hot site for any emergency treatment. These are patients who are possible or confirmed COVID-19 – including patients with symptoms, or those living in their household.
To enable our hub to see these patients we needed to do the following:
- Keep our patients and staff safe
- Follow correct infection control as stated by HTM 01-05 with the additional measures for COVID-19
- Ensure patient segregation
- Ensure adequate PPE
- Obtain fit testing certification.
Personal protective equipment
Sourcing the correct PPE was a challenge due to the massive increased demand from the hospitals. The main PPE difficultly was obtaining the appropriate masks and water resistant gowns for AGPs. The photograph below is a half face respirator, which can be used with P3 filters. These masks are reusable if cleaned correctly.

We also sourced Spectra Shield FFP3 masks, which are disposable after sessional use.

PPE for AGPs is as follows:
- FFP3 respirator/respirator with P3 filters
- Fluid resistant gowns
- Disposable gloves
- Visor (full face ideal)
- Bouffant cap.
The NHS has provided guidance on appropriate AGP for different settings and procedures within dentistry:
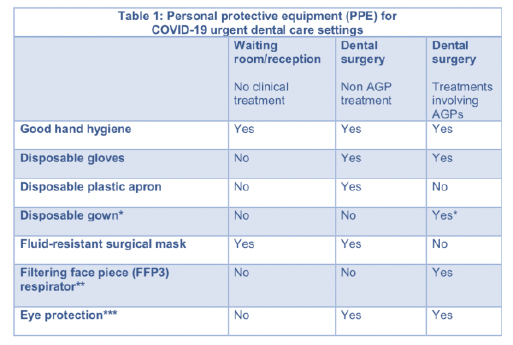 * Fluid-resistant gowns (or long-sleeved waterproof apron) must be worn during aerosol generating procedures (AGPs). If non-fluid-resistant gowns are used, a disposable plastic apron should be worn underneath. **If wearing an FFP3 that is not fluid-resistant, a full-face shield/visor must be worn. ***Eye protection ideally should be disposable. If polycarbonate safety glasses/goggles or equivalent are used, they should be disinfected in line with manufacturers’ guidance.
* Fluid-resistant gowns (or long-sleeved waterproof apron) must be worn during aerosol generating procedures (AGPs). If non-fluid-resistant gowns are used, a disposable plastic apron should be worn underneath. **If wearing an FFP3 that is not fluid-resistant, a full-face shield/visor must be worn. ***Eye protection ideally should be disposable. If polycarbonate safety glasses/goggles or equivalent are used, they should be disinfected in line with manufacturers’ guidance.

Consideration has to be taken when wearing the necessary PPE for AGPs. Until you have worked under these conditions it is hard to appreciate the potential difficulties, but these are some which we have identified:
- Increases in body temperature, especially as we are approaching the hotter months and air conditioning cannot be used. The clinical team must ensure that they are well hydrated
- Communicating with the patient and the rest of the dental team is more difficult because the masks muffle your voice, and lip reading is not possible
- Facial expressions are hidden, further hampering effective communication
- Poorer visibility
- More effort is needed to breathe
- Potential facial sores may develop with prolonged use.
Alongside the mask, other PPE is required depending on whether treatment is an AGP or not. If an AGP is to be undertaken, the clinical team will need to wear either a gown or apron and sleeves. We also included bouffant caps in our SOP. If there has been any doubt as to whether an AGP is to be performed or not, we have opted to don the PPE as if we were going to do an AGP, to cover all eventualities.
SOP (standard operating procedures)
We have to follow current guidance. Any SOP needs to be adapted by a practice that is intending to set up an emergency dental hub, so that it works on a local level. It also needs to be continually reviewed, so that it keeps up to date with the most current guidance. The model we decided to follow was to cluster several practices together, but each practice was still responsible for their own remote triage. From the initial contact, if the patient needed further treatment then the cluster practice could refer to the private urgent dental care hub.
The private urgent dental care hub then rings the patient and completes a COVID-19 risk assessment, medical history and history of the presenting condition. Following this, if face to face treatment is deemed appropriate, an appointment is booked for the patient.
Consent is important. Patients are made aware of the risk of catching COVID-19 as a result of attending the dental practice, and that the measures we have put in place are for their safety as much as the safety of the dental team. All patients are asked to park on the front drive way outside the practice and to ring the practice to say they have arrived. When the practice is ready to receive the patient, a ‘buddy nurse’ will meet the patient at the front door. The patient’s temperature is taken using a contactless thermometer and alcohol hand gel is dispensed into the patient’s hands.
The patient is reminded not to touch any door handles or railings. Social distancing will be maintained. Once the patient is with the clinical team in the surgery, the nurse will clean down handles and rails regardless of whether the patient touched them or not. The greeting nurse will be wearing disposable gloves, apron and a fluid-resistant type IIR surgical mask.
Points to note for initial contact
- Medical history and diagnosis are obtained through remote triage
- Only one patient is to be in the building at any one time
- Patients should attend their appointment alone unless they are unable to consent for themselves
- Appropriate COVID-19 risk assessment is carried out for each patient
- Patients do not enter the building until asked
- Patients are asked not to bring bags and coats into the practice if possible. They are also asked to go to the toilet before attending
- Temperature is checked at the door ensuring a temperature of no more than 37.8◦C
- Patients are advised not to touch anything such as door and hand rails etc.
Surgeries
The generation of aerosol as a result of dental treatment has garnered much interest during the pandemic, with speculation that it may be a factor in the spread of COVID-19. As a result, and following national guidance, our SOP was developed using the following principles:
- The surgery should be left empty for an hour following an AGP, meaning rotation of surgeries may be necessary to maximise available clinical time in the day. We decided to limit appointment slots to a maximum of six per day, although this may vary depending on the size of dental practice
- AGPs should be kept to a minimum
- Appropriate PPE must be worn for AGPs
- Strict protocols for donning and doffing PPE
- Surgeries cleared of all non-essential items
- The use of a ‘buddy nurse’ to escort the patient to and from the surgery, and to assist with provision of additional equipment, which may be required
- Surgery windows left open to facilitate air changes
- No air conditioning to be used, as this re-circulates the air and therefore may prevent the virus particles from settling
- Strict hand washing procedures.
Once the patient is in the surgery, no one should enter without the appropriate fitting PPE. Any anticipated instruments should be ready before the patient attends. On no account should the drawers in the surgery be opened. If an extra piece of equipment is required, the buddy nurse should be called to bring this to the surgery, passing it through the door. The buddy nurse will be wearing disposable gloves, apron and a fluid-resistant type IIR surgical mask. We found that keeping a trolley stocked up with items outside the surgery was a time-efficient way to implement this.
Cleaning
After the patient has left the surgery, the clinical team who treated the patient can then clear away any equipment used. Because it takes some time for any airborne virus particles to settle, the room should be left vacant for a period of time, with the windows open to promote air changes within the room. As an extra measure, we opted to use a fogger to aim to further reduce the viral load in the surgery.
After a period of one hour, the room can be re-entered by a member of staff who will then clean the room, including mopping the floor. They will be wearing gloves, an apron, a type IIR fluid-resistant mask and eye protection. Waste bags will need to be double bagged for disposal at the end of each session. To ensure the room is not entered before the hour is up, the buddy nurse writes the time the surgery was vacated on a board on the door.
Surgery windows should be left open during cleaning to increase the air changes in the room, and also prevent fumes from the cleaning chemicals from building up.
Safe management of laundry – scrubs at the end of a working session
Dirty scrubs can be put into a pillowcase or similar washable bag. These should then be washed at the highest temperature indicated on the garments, separate from other clothing.
Daily practice routine
To ensure all team members are fully aware of their roles and responsibilities, and to allow for changes in the SOP to be implemented quickly should the need arise (for example if guidance changes), we decided to hold daily practice meetings. We found that this also allowed staff members to raise any concerns that they may have, and as such the meetings were well received. The meetings also act as a refresher for staff training.
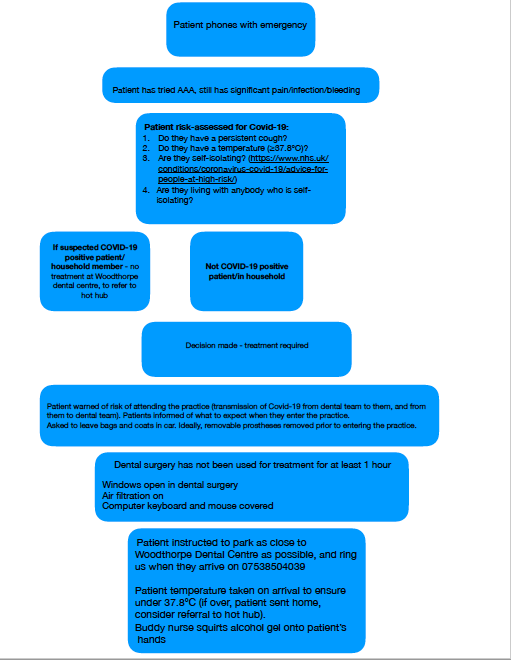
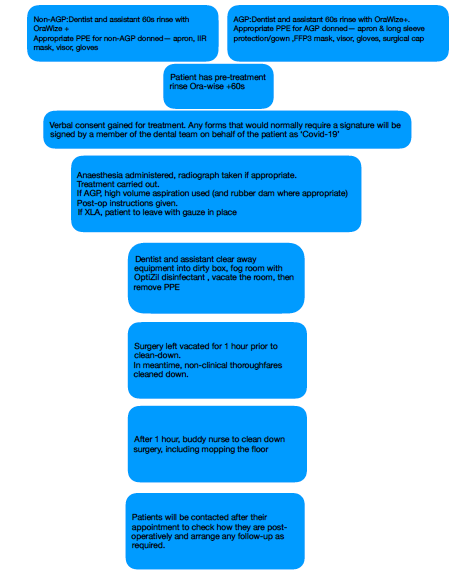
York private UDC COVID-19 protocol flowchart
What did we take into consideration when setting up the York private UDC?
Clinicians who may have dropped their working hours with their indemnity provider should ensure that they have adequate cover to work.
The CQC were informed of our intention to set up as a UDC. We also shared our SOP document with them. In addition we had to change our statement of purpose.
The creation of a cluster of practices is a key part in reducing the number of people potentially involved in face to face contacts. We organised fit testing for any dentist in the cluster who wanted it, and made it clear that they are able to see their own patients at the main site should they so wish. Those interested in undertaking clinical work were given a tour of the practice, and the SOP was discussed in detail with them. Each cluster practice provided a signed document from its lead clinician agreeing to the terms of referral to the hub. It was made explicitly clear that patients not usually seen at the main site are to return to their referring dentist for future care.
The nursing and reception staff completed CPD regarding COVID-19 as part of their training. Staff meetings were used to discuss the patient journey, telephone triage, and COVID-19 risk assessment. Documents such as the donning and doffing protocol and patient journey flowchart (Figure 1) were laminated and distributed within the practice.
Zoning of the practice was undertaken by the dentists, dental nurses and reception staff most familiar with the site. Several practice runs were carried out to make sure the patient journey was as efficient and safe as possible. Regular, open communication between the dental team allows for quick adaptation of the patient journey should a previously unforeseen issue come to light.
We have found, based on patient feedback, that a strong social media presence is beneficial. We have used social media as a platform to keep patients up-to-date with where dentistry currently sits within the pandemic. As well as using it to provide general dental advice. Patients have also been positive about the ease with which they have been able to speak to a member of the dental team. We feel it is essential patients are able to contact their own dental practice. Their own practice has access to information which may prove vital in aiding remote diagnoses (for example, if the patient had a recent deep filling).
What have we learnt so far?
Most of the work involved in setting up a private urgent dental care hub has been behind the scenes. Tailoring the SOP to an individual site and thinking through this novel patient journey benefits from input from all dental staff involved. However, there are a few key points which we have found require specific consideration:
- Excellent communication is needed over the telephone/video call, to ensure that the diagnosis is reached remotely as much as possible, thereby minimising the patient’s time in the surgery
- It is beneficial to inform patients what to expect on arrival. For example to stay in the car, go to the toilet before attending and how the clinical team will be dressed. The telephone conversation is the time to build rapport with the patient. This is very difficult to do when full PPE for AGPs has been donned. It is therefore important that one of the clinical team speaks with the patient prior to them arriving. There may not be a familiar face in the surgery, but at least there can be a familiar voice
- It is tiring and difficult to work in FFP3 masks. Talking and breathing are much more difficult. You can quickly feel uncomfortably hot, and the PPE can feel cumbersome
- In our experience, patients understand the importance of working under the restrictions of the COVID-19 pandemic. They understand their role in minimising face to face contact. And they understand their appointment may feel less relaxed and chatty than usual. Again, this is helped by the telephone conversation before the appointment
- Patients are really appreciative of being seen. This brings with it immense job satisfaction when we get them out of pain.
Conclusion
The York UDC was opened to treat patients in need. It was set up in a similar manner to the NHS hubs. Having a cluster with excellent communication between clinicians has enabled patients to be seen quickly, without any barriers to referrals.
Sharing information with other practices, fit testing together and generally sharing ideas have built a relationship with other local dentists, which we hope will continue into the future.
Remotely providing AAA remains the first line management of dental problems during the pandemic. However, issues such as pulpitis pain cannot be treated with antibiotics. A pulp extirpate is the treatment of choice if the patient does not want an extraction and analgesics are not helping.
Clustering local practices together helps to keep patient contact to a minimum. It is essential that the SOP keeps patient and staff safe.
The COVID-19 pandemic has changed all of our lives. At present nobody knows what the future holds for dentistry, especially in the short term. If we keep working together, keeping our patients’ best interests at the forefront of our minds, we will get through this.
 Kris Leeson is the practice principle of Thorpe Dental Group, based in York. He has an interest in dental implants and digital dentistry.
Kris Leeson is the practice principle of Thorpe Dental Group, based in York. He has an interest in dental implants and digital dentistry.
Rob Lewis is an associate dentist working at Woodthorpe Dental Centre on York. He is currently undertaking an MSc in periodontology.
Find out more about Dentistry’s Back to Practice campaign.



