In this Endodontics 101 column, Dr Sanj Bhanderi, past president of the British Endodontic Society, discusses minimally invasive endodontics, the microsurgery approach and the fundamental concept of modern endodontics.
Operating microscopes were introduced into the field of endodontics in the early 1990s. They are now the gold standard in current endodontic specialty and postgraduate programs in the UK.
They have become widely accepted and are an essential item of equipment used by specialist endodontists.
The advantages of utilising an operating microscope over magnification loupes include:
- Enhanced and co-axial light source (LED)
- Variance in magnification levels (x5 to x30)
- Ergonomics and working posture
- AV accessories for HD documentation and photography.
It is becoming more evident that the prognosis of implants isn’t always as predictable and problem-free as was initially purported. This is particularly true for multiple prosthetic units, and the remedy of implant-related disease can be costly and complicated.
Current research indicates healing and survival rates after apical microsurgery range from 89 to 94%. This is quite favourable and an acceptable outcome for most patients who wish to retain their teeth.
Minimally invasive (MI) endodontics
The fundamental concept of modern endodontic therapy is based on cleaning and shaping. That hasn’t changed for many years.
Achieving this goal with minimal damage to the tooth structure is the main challenge in endodontics. Endodontics is fundamentally the first stage in the restoration of an already compromised tooth and trying to save it by rendering it disease-free.
Therefore, the contemporary concept of MI dentistry also applies in endodontics throughout all stages of treatment. It includes:
- Conservative access preparation
- Judicious removal of infected/affected pulp tissue
- Identification and entry into the pulp canal space
- Disinfection (mechanical and chemical)
- Debridement
- Removal of ‘smear layer’
- Filling and sealing the pulp space as completely as possible
- Effective and stable coronal seal.
It is evident that any breaches or shortcomings at any stage of this process will eventually lead to failure. This could result in recurrent or persistent pathosis in the supporting periodontal tissues, tooth fracture, ongoing symptoms, and potential tooth loss.
Surgical approach
In routine dental practice, the above clinical approach usually applies to conventional (orthograde) endodontic treatment via a coronal approach.
However, the same concept is equally important if a surgical approach is to be considered to deal with a failing endodontic case, albeit with a direct approach towards the root-ends and apical tissues.
The MI approach includes managing both soft and hard tissues with equal care, under high-power microscopic magnification, and employing microsurgical principles and instruments. Hence, we now consider the traditional ‘apicectomy’ procedure as apical microsurgery.
The key to successful surgical treatment is in the diagnosis, planning, and execution of the procedure:
- Obtaining a thorough clinical history, evaluation of the affected tooth in terms of coronal seal, periodontal health, and assessing patient motivation
- CBCT evaluation of the affected tooth for correct diagnosis and identification of the causative factors for the endodontic failure
- Careful soft tissue management (conservative flap design) to minimise intra- and post-operative complications
- MI hard tissue management to minimise post-operative complications, for root preservation, whilst allowing for adequate disinfection and obturation.
There are multiple indications and contraindications for endodontic microsurgery. All of them must be carefully ascertained as they will often dictate the reason (or not) to perform the surgical procedure.
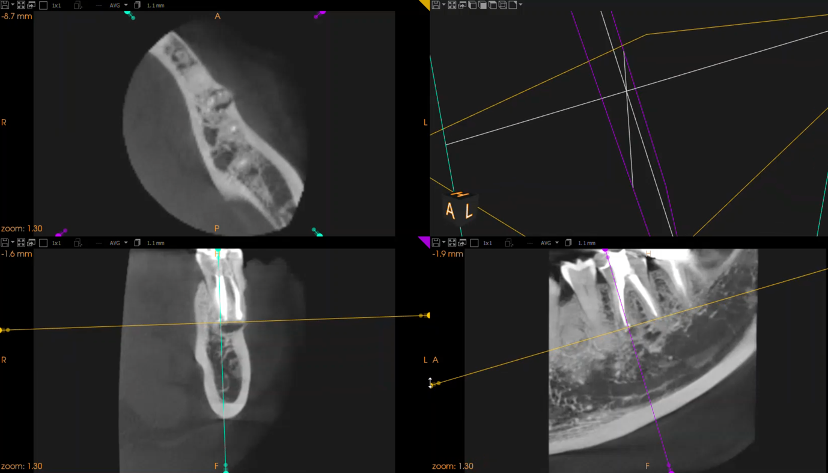
Small-field CBCT (Figure 1) scanning of the affected teeth is now an essential tool for pre-surgical planning. This is for the following reasons:
- Identification of iatrogenic defects
- Identification of missed roots/pulp space that will require preparation and sealing
- Size, position, and margins of the endodontic lesion
- Proximity of important anatomical structures, which may be affected by the surgical procedure (eg neurovascular channels, sinus spaces, etc).
The surgical procedure
Flap design
Currently, the two flap designs that are favoured by the author are:
- Base of papilla incision (Figure 2a)
- Submarginal incision (Figure 2b).
Both designs can be completed with a single or double relieving incisions.
Microsurgical blades are necessary in order to incise with clean precision.
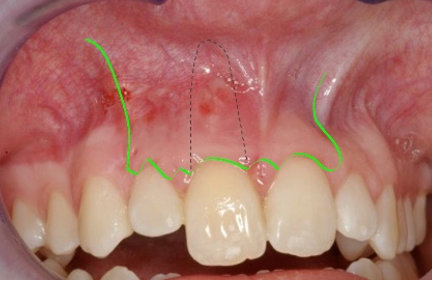
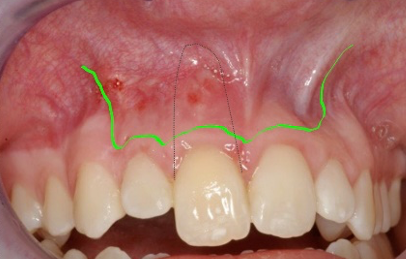
Both flap designs have the advantage of maintaining the integrity of the interdental gingival papillae to prevent marginal recession. This is a concern for many patients in the aesthetic (anterior) zone.
Another benefit of these flap designs is good soft tissue healing with minimal postoperative complications.
Recommended sutures are of a 11mm semilunar reverse-cutting needle, 5/0 or 6/0 grade prolene/PTFE/Polyglycol material which should be removed three to five days after the insertion.
Osteotomy and apical resection
With the ethos of an MI approach, the size of the osteotomy should be based on the CBCT scan. The osteotomy to access the infrabony lesion should be as conservative as possible.
Gentle action of surgical high-speed surgical turbine tungsten carbide bone-cutting burs, or ultrasonic (piezo) devices (Figure 3) can be used to access through the cortical bone.
The contemporary method for MI osteotomy is a ‘targeted’ approach. This can be achieved in two different ways:
- Using a 3D-printed guide and custom-designed bone drilling burs devised based on the preoperative CBCT scan. (Similar method is currently used by implant surgeons to guide implant placement)
- Dynamic CBCT guided approach with real-time navigation of the bone burs and handpiece held by the surgeon (NAVIDENT system).
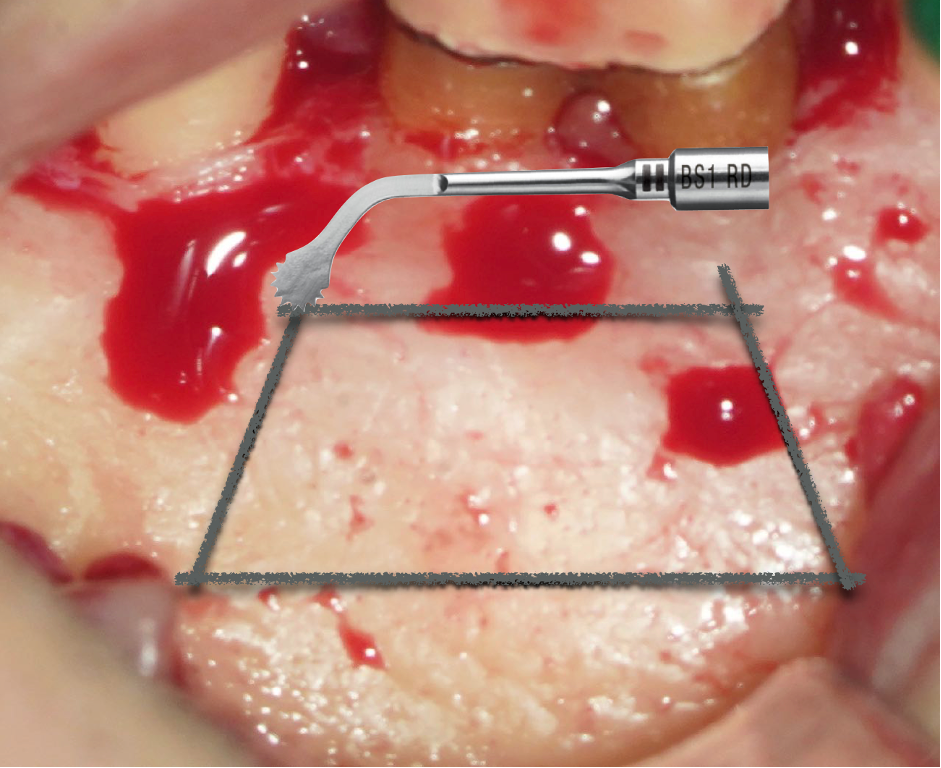
Retrograde preparation
The essential endodontic process of ‘cleaning and shaping’ of the infected pulp canal space(s) can then be performed using retrograde ultrasonic tips (Figure 4).

Currently, these tips are available in 3mm, 6mm, and 9mm lengths which allow for cleaning of a significant length of canal space if necessary.
Sealing (obturation) the pulp space
After retrograde preparation of the pulp space, it must be sealed to prevent re-percolation of residual biofilm and for long-term stability and healing (Figure 5).
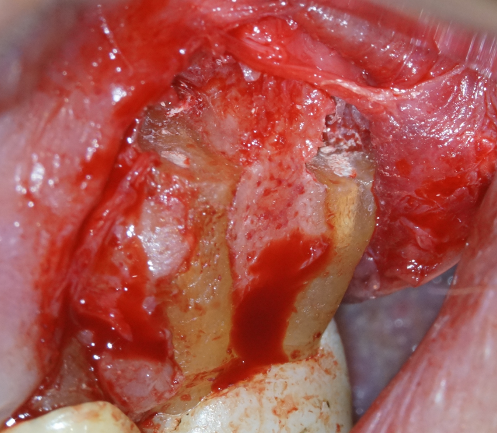
Contemporary materials developed from original MTA are ‘hydraulic’ (calcium silicate) putty materials. They are favoured because they are hydrophilic and set in the moist surgical environment, and also because of their alkaline setting properties, which is conducive for rapid bone healing.
The past 20 years has seen a dramatic advancement in different areas of endodontics, such as biological concepts, science of dental material and technology. These advancements have enabled us to offer an opportunity to save heavily restored and root-filled teeth that, hitherto, would have simply been extracted due to the increasing popularity of implant placement.

Even in teeth that are endodontically compromised but are restoratively stable and have an opportunity for survival, surgical endodontics gives an option to maintain such teeth, at least until the patient is ready to have it extracted and consider a dental implant in the future.
With the correct conditions in restoratively stable teeth, apical microsurgery is a viable alternative that should be offered to motivated patients to try and save their teeth (Figure 6 and 7).

Email [email protected] for references
Catch up on the last Endodontics 101 article:
Follow Dentistry.co.uk on Instagram to keep up with all the latest dental news and trends.


