 In this month’s guide, Hannah Hook looks at the pre-operative assessment of mandibular third molars.
In this month’s guide, Hannah Hook looks at the pre-operative assessment of mandibular third molars.
Extraction of mandibular third molars (M3Ms) has progressively become an increasingly common procedure.
However, despite this, it carries various associated risks. And whilst some of which are considered relatively minor and infrequent, the severity and incidence can vary significantly (Al Ali and Jaber, 2020).
In 2000, NICE guidance for the extraction of wisdom teeth was released. But this is now over 20 years old and more research in this field has since been undertaken.
More recently, in 2020, the Royal College of Surgeons of England (RCSEng) released updated guidance on the assessment of M3Ms. This was produced in response to evidence suggesting there is an increasing level of patient harm due to the retention of M3Ms.
Initial assessment
The assessment of M3Ms starts with a thorough assessment of the patient’s medical and dental history. This aids in triaging the patients based on urgency.
Clinicians should ask patients if they have had any symptoms associated with their M3Ms; such as pain (number of episodes and severity), swelling and limited mouth opening.
You should also complete an extraoral assessment, assessing for signs of infection, such as oedema, erythema, or lymphadenopathy.
M3M assessment
Following this comes clinical examination of the M3Ms:
- Eruption status – unerupted, fully or partially erupted
- Their position in relation to the mandibular second molar
- If they are functional
- Their place in the occlusion
- Associated periodontal disease
- Opposing maxillary third molar
- Oedema, erythema.
Radiographic assessment
Radiographs allow gathering of further information on the size, shape, and position of the M3M. Along with the presence or absence of disease within the tooth or surrounding area (Royal College of Surgeons of England, 2020).
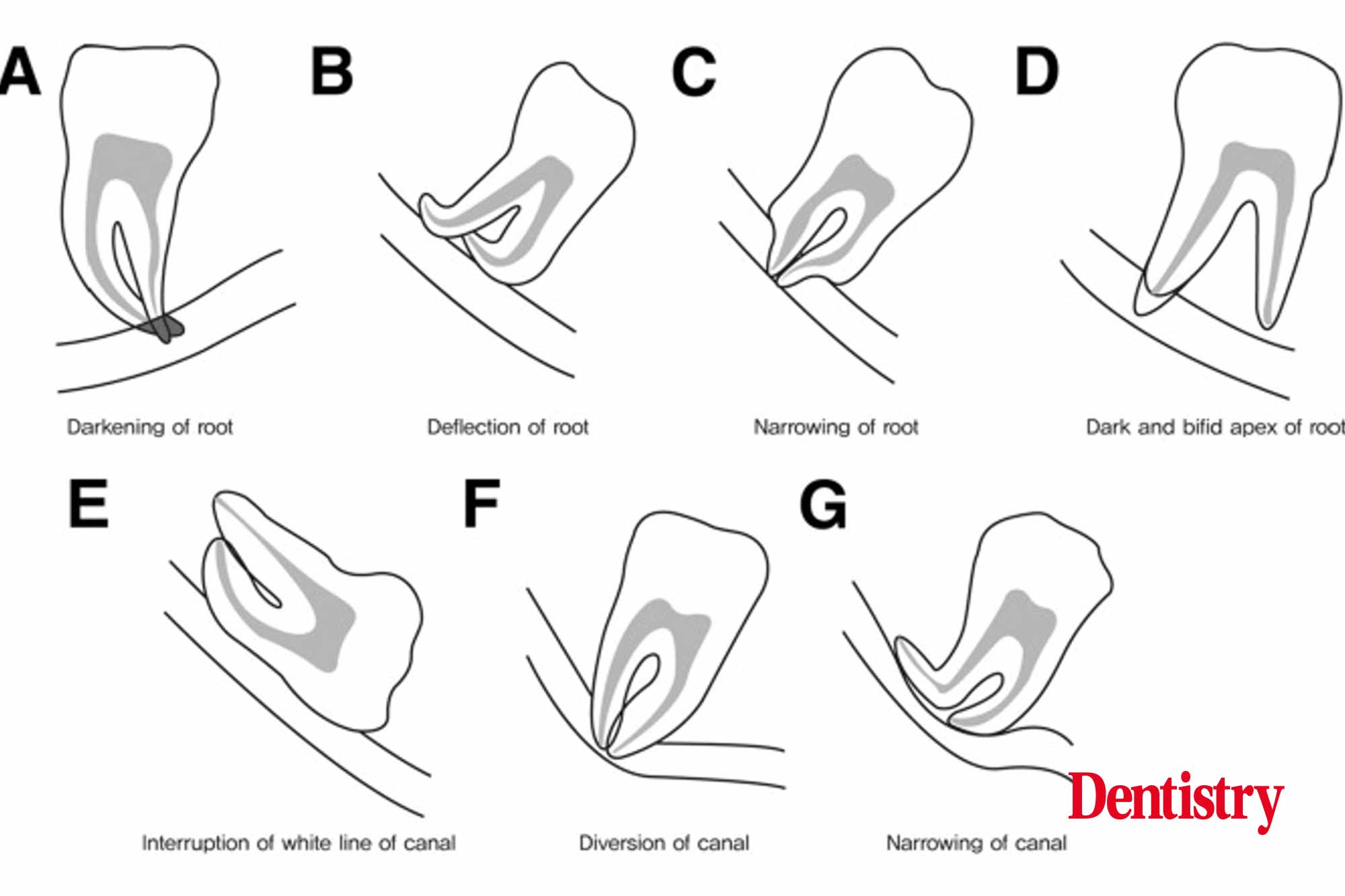
An orthopantomogram (OPT) is the standard imaging technique for the assessment of M3Ms. It enables assessment of the M3M in relation to the inferior alveolar nerve (IAN). The radiological signs that a M3M is close the IAN (Figure 1) include (Al Ali and Jaber, 2020):
- Darkening of the root
- Deflection of the root
- Narrowing of the root
- Dark and bifid apex of root
- Interruption of the white cortical line
- Diversion of the IAN canal
- Narrowing of the canal.
The 2020 guidance by the RCSEng suggests that cone beam computed tomography (CBCT) is of use when conventional radiographic imaging shows a close relationship between the M3M and the IAN.
CBCT can help show if there is direct contact between the IAN canal and the M3M. Or whether there is bony separation between them (Royal College of Surgeons of England, 2020).
Indications for extraction
Guidance from the RCSEng (2020) suggests that the ‘Practice of prophylactic removal of third molars should be discontinued in the NHS’.
Therefore, we should restrict surgical removal of M3Ms to patients with evidence of pathology, such as the following (Royal College of Surgeons of England, 2020):
- Unrestorable caries
- Periodontal disease of M3M or second molar
- Non-treatable pulpal and/or periapical pathology
- Cellulitis
- Abscess
- Osteomyelitis
- Internal or external resorption of the tooth or adjacent teeth
- Fracture of tooth
- Disease of follicle including cyst or tumour
- M3M is in the surgical field.
A patient who has only experienced one episode of pericoronitis (unless extremely severe), should not be considered as an indication for surgery (Royal College of Surgeons of England, 2020).
Winters lines
Winters lines classification provides an assessment of the degree of difficulty of extraction of a M3M. It comprises of three lines, red, amber, and white. These are superimposed onto a radiograph (Figure 2).
White line
- Drawn across the occlusal surface of the mandibular molars extending posteriorly over the M3M
- The white line signifies the difference in the occlusal level of the first, second and third molars.
Amber line
- Represents the height of the bone level
- Shows the amount of bone overlying the M3M
- Indicates how much bone removal is required.
Red line
- Drawn perpendicular from the amber line to an expected point of application of an elevator
- If mesially impacted, then this is usually the cemento-enamel junction (CEJ) on the mesial aspect of the M3M. If distally impacted, then the CEJ on the distal aspect
- The red line highlights how much bone will need removing to allow elevation of the tooth
- As the red line increases by 1mm in length, the difficulty of extraction is three times more
- If the line is less than 5mm in length then removal under local anaesthetic is appropriate. Anything above 5mm may require sedation or a general anaesthetic.
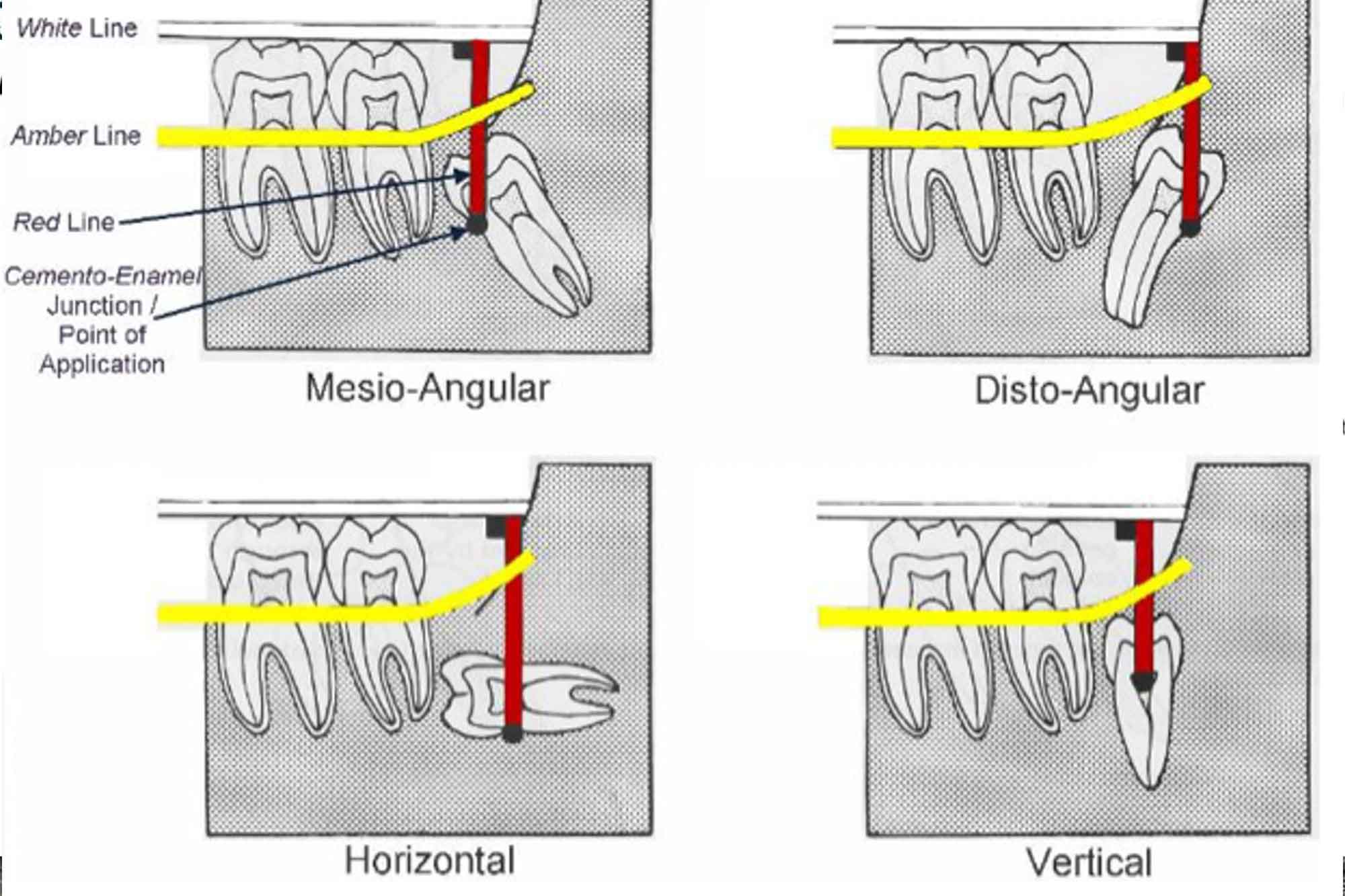
Figure 2: Displaying Winters lines
Factors increasing the difficulty of extraction
- Disto-angular positioning
- Long thin roots
- Divergent roots
- Narrow periodontal ligament space
- Close relation to the IAN
- Close relation to the mandibular second molar
- Dense bone.
Coronectomy
If M3Ms are in very close proximity to the IAN and therefore extraction poses a high risk of nerve damage, an alternative method for management is coronectomy.
Another indication for coronectomy is if there is hypercementosis of the M3M (Royal College of Surgeons of England, 2020). However, the criteria for patient selection is strict. This is due to the risk of possible infection, pain and requirement for future removal of the roots. Contraindications include (Royal College of Surgeons of England, 2020):
- Non-vital M3M
- Caries with a high risk of pulpal involvement
- Mobile M3M
- M3M with associated apical infection.
Key points
- Carry out a thorough initial assessment of the patient, including their medical and dental history
- Radiographic assessment with an OPT allows visualisation of the IAN and assessment of the M3M proximity to the canal
- There are several signs that a M3M is close to the IAN
- If a M3M is deemed to be in close proximity to the IAN then a CBCT is useful in determining whether there is a direct connection between the IAN canal and the M3M
- Prophylactic removal of M3Ms should be discontinued
- Winters lines provide a method for assessing the difficulty of extraction of M3M
- Coronectomy is an option for M3Ms where extraction is very difficult (hypercementosis) or poses a very high risk of nerve damage.
References
Al Ali S and Jaber M (2020) Correlation of panoramic high-risk markers with the cone beam CT findings in the preoperative assessment of the mandibular third molars. J Dent Sci 15: 75-83
Royal College of Surgeons of England (2020) Parameters of care for patients undergoing mandibular third molar surgery
Catch up with previous Student’s guide
- Luting cements
- Pregnant patients
- Impression materials
- Common medications (part three)
- A dental student’s guide to…common medications (part two).
Follow Dentistry.co.uk on Instagram to keep up with all the latest dental news and trends.


