 In the wake of the 70th anniversary of the NHS, Roger Matthews considers the impact this beloved institution has had over the years on dentistry in the UK.
In the wake of the 70th anniversary of the NHS, Roger Matthews considers the impact this beloved institution has had over the years on dentistry in the UK.
Dentistry in the UK is awaiting reform. The BDA complains that there is simply not enough state funding and there is a looming recruitment crisis. Dentists are not kept informed of progress. Rampant government bureaucracy is stifling patient care.
Sound familiar? Wait, it’s…February 1948.
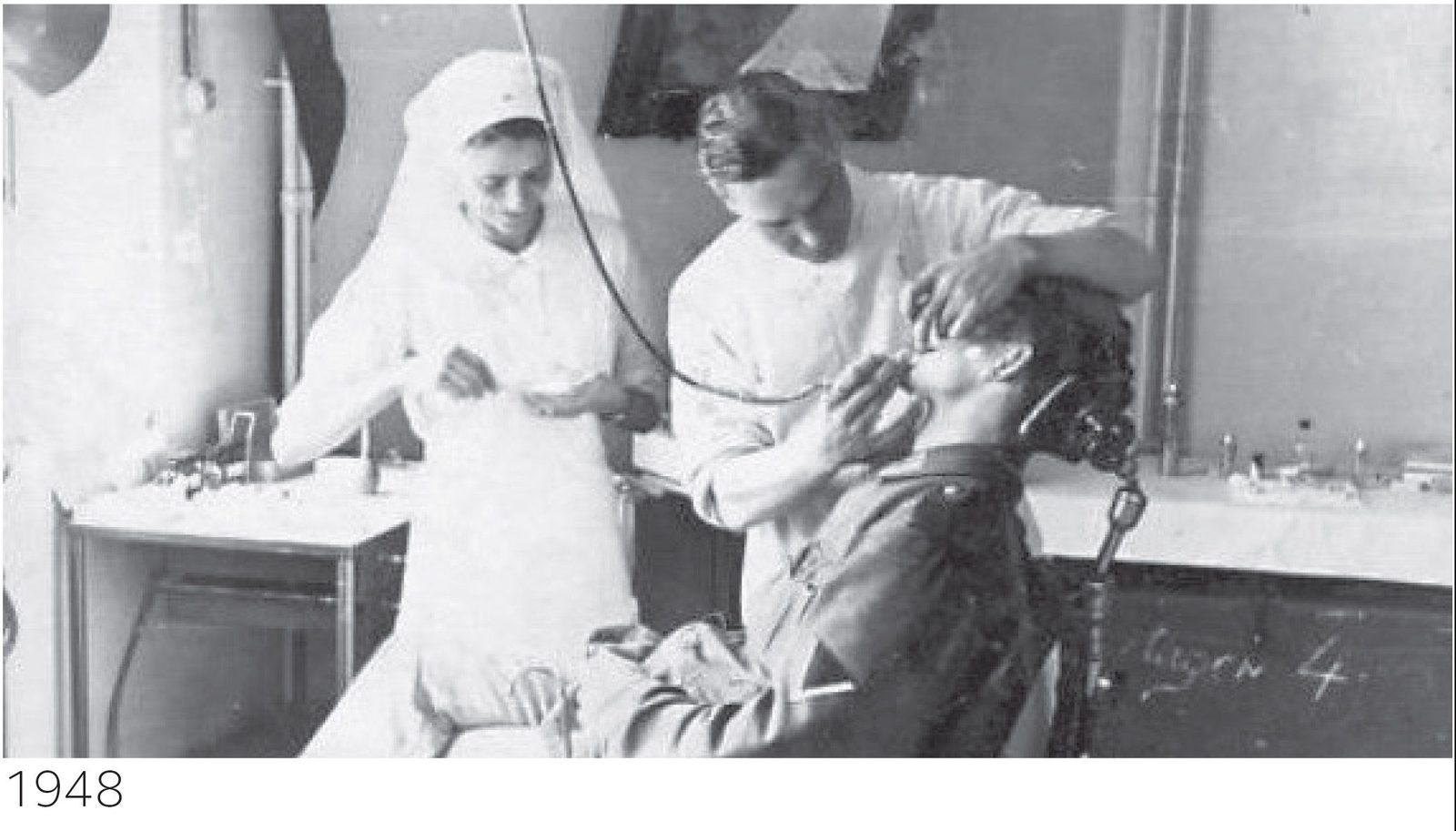
Dentists’ waiting rooms had been deserted for two years, since the passing of the NHS Act in 1946. The population was determined to wait for their ‘free treatment and dentures’. That population, recovering from war, was 50 million. Life expectancy for men was 65 years; the average house price was £1,750; the average yearly income for a teacher was £600; dentists’ income was around £1,400 (and falling rapidly); a pint of milk was 2p, a pint of beer 7p.
In February 1948, less than five months before ‘the appointed day’ on which the NHS would be launched (Monday 5 July), the BDA was arguing strenuously that dentists should not sign up to the ‘inflexible and intransigent’ demands of the Minister, Nye Bevan. Other, smaller dental groupings, including the ‘unqualified’ 1921 cohort of dentists who had undergone apprenticeships, were divided.
Complicated scale of fees
The BDA argued that it had had only three weeks to agree to a ‘complicated scale of fees’, and indeed by July, most dentists had still not received their papers to enrol because ‘the bureaucratic machinery had creaked to a standstill’ – shades of Capita, perhaps?
Nevertheless, the money was generous, and by the end of 1949, 94% of dentists had signed up to provide NHS services. So huge was the pent-up demand (more than 70% of adults were edentulous and 80% of 12-year-olds had ‘significant decay’) that in its first year, dentistry even outspent GP services and hugely overshot its budget.
Government response was swift. In February 1949, fees were cut by 50% for dentists earning more than £4,000, and in May of that year, Bevan told the Cabinet: ‘The dentists soured public opinion by their behaviour. I allowed them to misbehave to get the atmosphere for cuts. I am now cutting fees – by 40%’.
Clawback indeed – with a vengeance!
In fairness, many dentists employed salaried assistants, which simulated high incomes, so the self-employed ‘associate’ was created, each with his own contract (there were very few female dentists).
All that was 70 years ago, and there have been many milestones – and stumbling blocks – along the way. Bevan himself resigned from the Government in 1951 when dental charges (of £1) were introduced, first for dentures, and the following year for treatment. Prices for dentures rose, but the £1 fee remained until 1971.
By 1976, the routine charge had risen to £3.50 (with a maximum of £12); those costs have gone up inexorably and today the routine fee in England is £21.60, with a maximum of £256.50. For a number of dentists, the routine patient fee now exceeds their NHS tariff!
What else has changed? Bread was still rationed when the NHS began, and sugar remained so until 1954. Disease levels remained high and edentulousness only began to decline steeply in the 1980s (to less than 6% today). Fluoride toothpaste appeared in 1958, but not until Procter & Gamble introduced Crest in the early ‘70s did it become mainstream.
Low patient charges, the wide availability of NHS dentistry, and the introduction of the high-speed air rotor in 1957 combined to accelerate the ‘heavy metal generation’, which persisted for three decades.
Healthcare has changed beyond all recognition over the 70 years of the NHS. In 1948, the principal causes of mortality were rheumatic heart disease, respiratory illness and infection; today, they are heart disease, cancer, and dementia. Rickets and poliomyelitis were prevalent in the early years and vaccinations were in their infancy. Indeed, ‘prevention’ was largely unknown.
GDC created
The dental profession, too, has evolved; it was only in 1956 that the General Dental Council was created, freeing dentists from the oversight of their medical colleagues. There are now more than twice the number of practising dentists relative to the population.
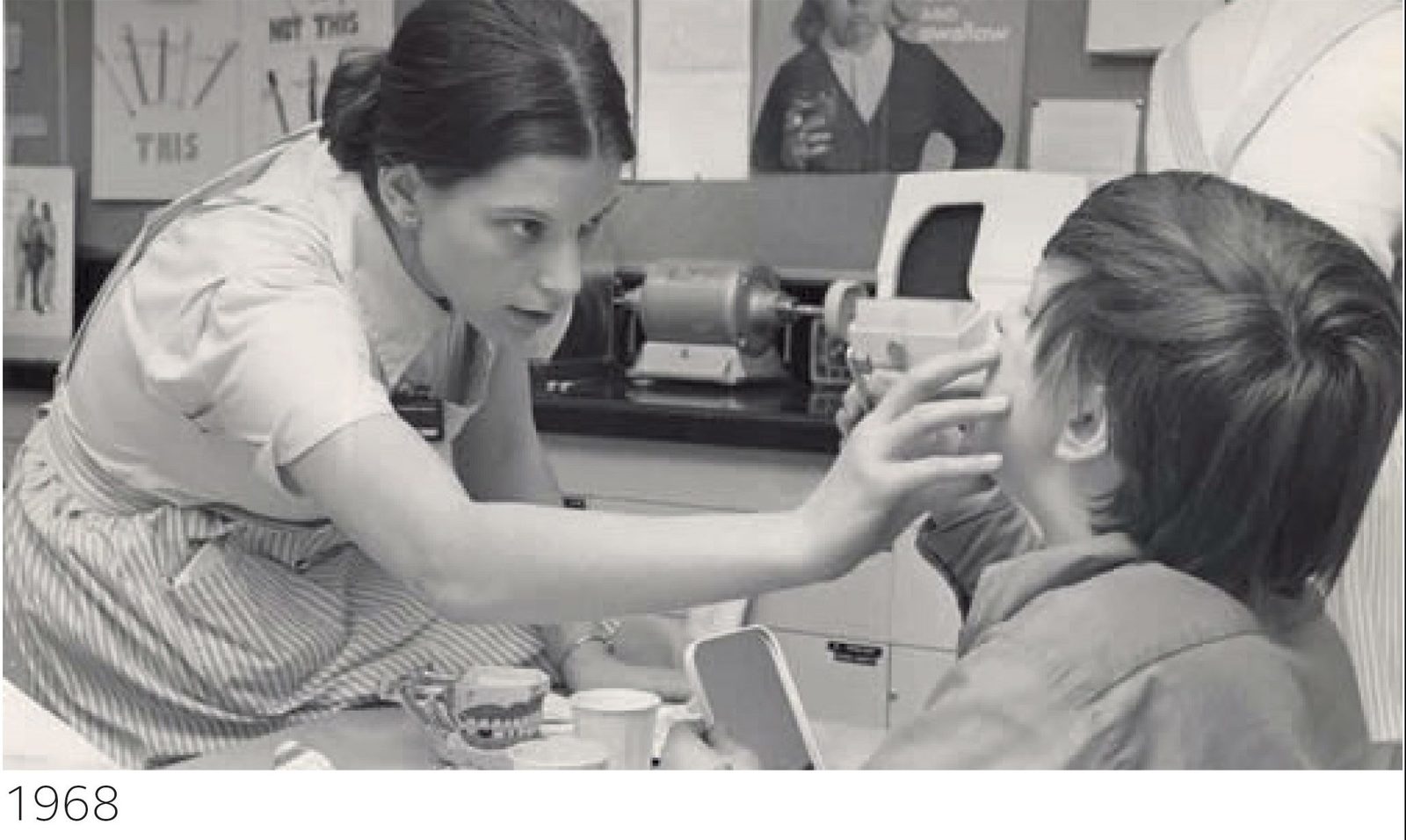
Dental hygienists were trained by the RAF during World War II and were officially licensed to practice by the 1957 Dentists Act. Dental auxiliaries (first introduced in New Zealand in 1920) began work in local authority clinics in 1961, becoming dental therapists in 1979. It took another 20 years before they were permitted to work in general practice.
The NHS General Dental Services continued to work under a complex fee-per-item basis from 1948 until 1990. The Dental Estimates Board employed over 2,000 clerks in Eastbourne to process paper claims from dentists and give ‘prior approval’ to most complex treatment, including crowns, bridges, inlays, and metal dentures (even for more than four X-rays in 1948!).
Fee levels were a constant bone of contention between the dentists and the Government. The Pilkington Report of 1960 recommended that an independent group – the Doctors’ and Dentists’ Remuneration Body – be set up and that fee-per-item should continue, but with a target net annual income, set by the Dental Rates Study Group.
Prevention and capitation
In 1964, the BDA commissioned the Tattersall Report, which proposed a move to capitation, (similar to GPs) but this was not approved. However, for the first time, the concept of ‘prevention’ of disease became current and after negotiation, a hybrid capitation, registration and fee-per-item NHS contract was agreed in 1990. Once again, the profession overspent the Government’s planned budget and a clawback of 7% of fees took place in 1992.
In the meantime, of course, Stephen Noar had been experimenting with a private capitation scheme in his Reading practice and, in 1986, Denplan was born! The timing was excellent, since the 1990-92 debacle resulted in many dentists phasing down or exiting the NHS.
Of the current contract, little needs to be said here to add to the criticism already levelled by Parliament, patient groups, and the profession itself. Times have changed and it is perhaps ironic that the Commons Health Select Committee in 2007 described the management of dentistry by the state as one of ‘supervised neglect’.
Seventy years is a long time to sustain an uneasy relationship, however well-intentioned.


