 Andrew Osafo reviews vital tissue staining, chemiluminescence and autofluorescence as aids to mouth cancer screening.
Andrew Osafo reviews vital tissue staining, chemiluminescence and autofluorescence as aids to mouth cancer screening.
As dental professionals, we are in a prime position to educate the public about mouth cancer. Are you doing this?
Mouth cancer is a serious and debilitating disease that can devastate lives – and prematurely end them.
The Mouth Cancer Foundation recommends dental professionals carry out a mouth cancer screening on every patient over the age of 16 at least once a year.
Dr Ciro Gilvetti and myself also wrote an article about how to perform a comprehensive mouth cancer examination.
According to the Oral Health Foundation, early detection of mouth cancer results in a 90% survival rate. Compared to 50% in late detection of mouth cancer.
Unfortunately, we diagnose approximately half of all mouth cancers at advanced stages (stages III or IV) (Gómez et al, 2009). By these stages, the treatment required is for a systemic disease process. Rather than a localised condition, as a result of lymphatic spread.
Detecting mouth cancer at the early stages is difficult. Abnormal lesions may not be palpable and also the colour of these lesions are not dissimilar from the surrounding mucosa.
Therefore techniques have been developed for use in conjunction with a mouth cancer examination to improve the detection of early malignancy.
This article reviews the following adjunctive techniques: vital tissue staining, chemiluminescence and autofluorescence.
Vital tissue staining
Vital staining is the process of staining living cells or tissues. Tolonium chloride (Toluidine blue) is a metachromatic vital dye. It has more than 40 years use aiding the detection of mucosal abnormalities of the cervix.
Toluidine blue has a high affinity for acidic tissue components. Consequently it selectively stains tissues that are rich in RNA and DNA (Sridharan and Shankar, 2012).
Pre-malignant and malignant cells contain significantly more RNA and DNA compared to normal cells. Therefore areas stained dark blue (a positive stain) require further investigation.
The Orablu Oral Lesion Marking System (Addent Inc) contains three components:
- Tolonium chloride
- Acetic acid
- Applicator swabs.
Apply acetic acid to the tissues by means of applicator swabs before and after applying tolonium chloride. The acetic acid helps to remove surface debris.
The test is considered positive if the dye is retained following the application and de-staining with acetic acid.
Chemiluminescence
Chemiluminescence or tissue reflectance has been used in gynaecology and obstetrics to detect premalignant and malignant lesions. This technique has therefore been adapted for use in the oral cavity.


Use chemiluminescent light to assess the oral cavity after rinsing the mouth with acetic acid. Applying acetic acid results in surface coagulation of cellular proteins and dehydration of the cells. This then reduces the transparency of the epithelium.
Malignant cells have increased light reflectance compared to normal cells. They have a higher nucleus to cytoplasmic ratio.
Under blue-white illumination, abnormal cells appear white (acetowhite). While normal cells appear bluish because these cells absorb light (Figure 1).
The Microlux Transilluminator 2 (Addent Inc) is a multipurpose device that can screen for caries, fractures and oral mucosal abnormalities. The unit consists of a high-intensity light emitting diode (LED) fibre optic source.
The transilluminator has various attachments designed for different applications.
When a Microlux Diffused Light (DL) guide is attached to the transilluminator a blue-white light (65,000K) is generated. This helps to visualise mucosal abnormalities (Figure 2).

Autofluorescence
Cells and tissues contain molecules called fluorophores.
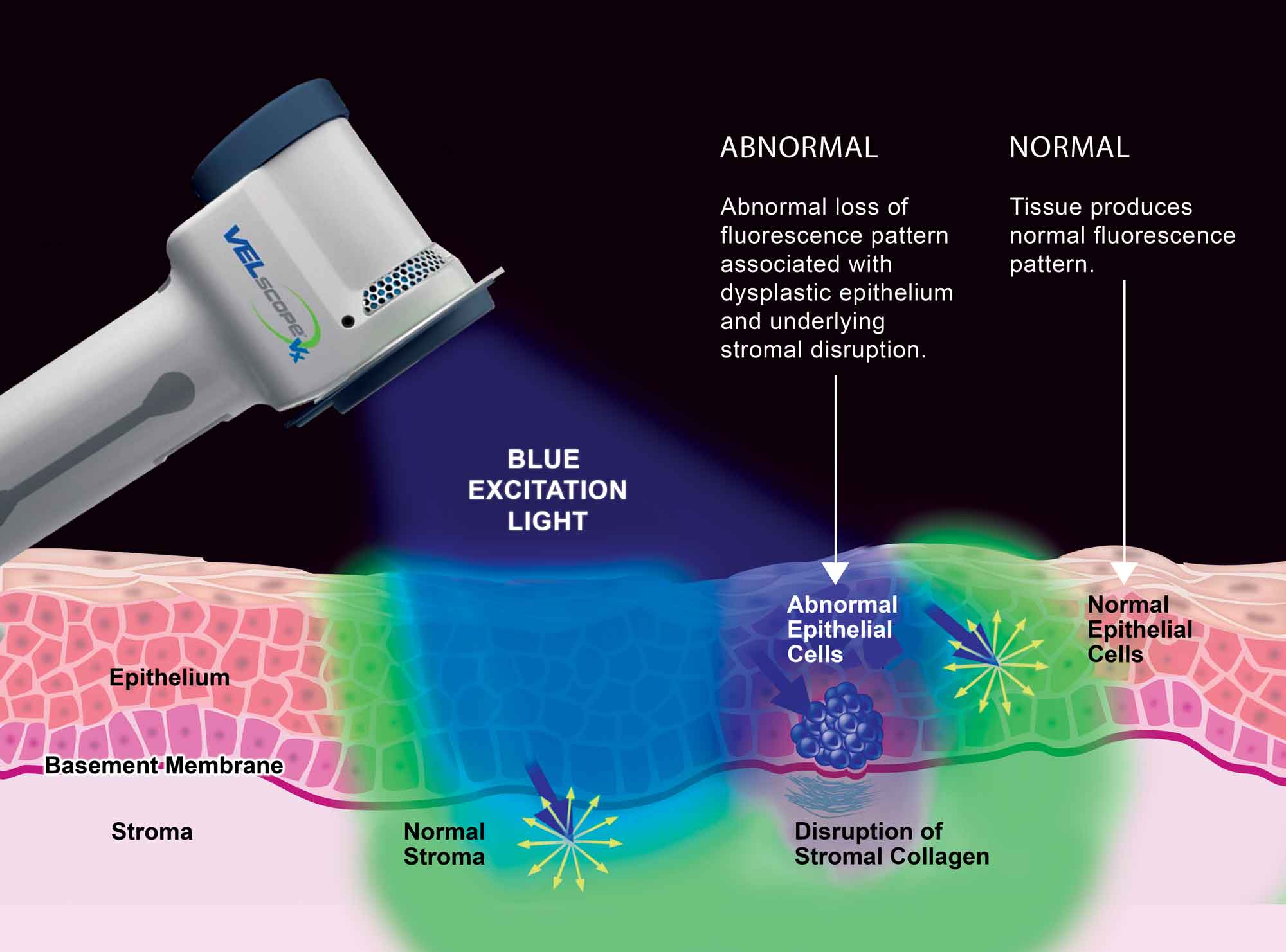
When light of a specific wavelength (blue/violet light, 400-450 nanometres) excites fluorophores, they will emit their own light at a longer wavelength (green light). This phenomenon is known as autofluorescence.
Loss of tissue autofluorescence is associated with malignant and pre-malignant lesions.
Cells and tissues are viewed through optical filters that allow the passage of long wavelength red and green autofluorescence. Typically, healthy tissue appears green (emits fluorescence) while abnormal tissue appears dark (Figure 3).
Autofluorescence devices are useful for detecting lesions we do not easily notice by visual inspection and do not require the use of rinses or lesion-marking solutions (Figure 4). Many studies look at the use of autofluorescence devices to detect oral mucosal abnormalities (Tiwari L, Kujan O and Farah CS, 2019).

Detecting autofluorescence
To effectively use these tools, it is important to know how normal phenomena appears when viewed through an optic filter.
I would recommend anyone reviews the education support material for autofluorescence devices on the Apteryx imaging website.
The Velscope (which stands for visually-enhanced lesion scope) was the first autofluorescence device for dentistry. The latest model is a cordless non-magnifying device called the Velscope Vx (LED Dental Inc).
Velscope VX has a blue light source integrated into the handpiece and has an optical viewing filter. The Velscope Vx Imaging Adapter is also an optional accessory available that allows fluorescence and normal white light reflectance image acquisition (Figure 5).

The Bio/Screen Oral Examination Light (Addent Inc) is a biofluorescence screening device. Clinicians can use the device in full room light due to having five high-power violet LEDs (Figure 6).

SLR camera and phone adapters are available for the Bio/Screen Oral Examination Light to take clinical photographs.
The GOCCLES (Glasses for Oral Cancer – Curing Light Exposed – Screening) device (Pierrel Pharma Srl, Italy) is one of the latest autofluorescence systems.
The GOCCLES device provides an easy and low-cost method to visualise oral mucosal abnormalities. The system consists of a pair of glasses with filters highlighting autofluorescence when light from any dental curing light illuminates mucosa.
The GOCCLES device allows binocular vision and does not need any consumable products to function (Figure 7).

Suspicious areas
If you discover unusual findings during the examination, clinicians should make a review appointment two weeks after the initial examination.
Record the size, shape, colour, texture and position of the suspicious areas. It is also a good idea to take clinical photographs of the area of concern.
The oral mucosa generally heals itself in two weeks. So if the suspicious areas are still present at the review appointment, refer the patient for further investigation.
Refer highly suspicious lesions (Figure 8) urgently under the ‘two-week wait’ referral pathway. A biopsy and a histopathological examination are necessary to diagnose a suspicious lesion.

Conclusion
Early detection and diagnosis of mouth cancer dramatically improves survival rates. It also makes treatment and rehabilitation easier.
Adjunctive techniques assist healthcare professionals to detect oral mucosal abnormalities. These tools do not replace or diminish the mouth cancer clinical examination. But rather should complement and strengthen existing clinical protocols. They also do not provide a diagnosis.
As with any new technique or technology, there is a learning curve. Therefore professionals need to invest the time to learn how to use them effectively.
Systematic and regular screenings save lives. Consequently, as healthcare professionals, are we doing our part to raise awareness of mouth cancer?
For further information on how to screen for head and neck cancer, visit the Mouth Cancer Foundation’s website at www.mouthcancerfoundation.org/get-info/screening-head-and-neck-cancer.
References
Gómez I, Seoane J, Varela-Centelles P, Diz P, Takkouche B (2009) Is diagnostic delay related to advanced-stage oral cancer? A meta-analysis. Eur J Oral Sci 117(5): 541-6
Sridharan G, Shankar A (2012) Toluidine blue: A review of its chemistry and clinical utility. J Oral Maxillofac Pathol 16(2): 251-5
Tiwari L, Kujan O, Farah CS (2020) Optical fluorescence imaging in oral cancer and potentially malignant disorders: A systematic review. Oral Dis 26(3): 491-510
This article first ran in Dentistry magazine. You can also read the latest issue of Dentistry magazine here.
You can also follow Dentistry.co.uk on Instagram to keep up with all the latest dental news and trends.


